PSYCHOSOCIAL COGNITIVE DYSFUNCTION IN SCHIZOPHRENIA
Abstract
Introduction: Features of schizophrenia identified in the literature: the most severe and disabling psychosis; chronic disease with poor development potential; heterogeneity; multifactoriality; multidimensionality; high variability among cultures and regions. Objectives: To verify the possibility of identifying and assessing the cognitive deficits of patients with a diagnosis of schizophrenia through cognitive tests; assessing changes in cognitive functioning in patients with schizophrenia who received treatment with antipsychotic drugs. Material and Method: To achieve work objectives there were used: Rating Scale positive symptoms, negative and disorganization (Scale - PANSS, Stanley, Lewis and Abraham, 2006); a battery of tests designed to measure the constructs and cognitive functions commonly disturbed in schizophrenia. The study included a group of 55 patients diagnosed with schizophrenia. Results: There is a significant relationship between clinical symptom scores evaluated by the PANSS Scale, performance on tests that evaluated the cognitive functions and efficacy of atypical antipsychotic drugs. Conclusion: In schizophrenia there is a deterioration of cognitive activity, which is possible evidence of specific psychological tests. Maintaining the correlation coefficients values relative to the same level as in the initial assessment shows that cognitive deficits manifested in terms of negative symptoms are more resistant to change under treatment with antipsychotic use.
Schizophrenia is the most severe and disabling psychosis, a chronic disease with a poor evolutionary potential (1). Other main features of schizophrenia are heterogeneous, multidimensional, multifactoriality.
Symptoms of schizophrenia are arranged into groups or clusters called domains. The domains of dysfunctions are positive symptoms, negative symptoms, cognitive impairments, mood and suicidity, and aggression (2). The pattern of dysfunction in different domains is independent and varied in etiology, pathogenesis, and their response to treatment. Positive symptoms include new behaviors generated by neuropsychological system like disorder of thought, delusions, hallucinations, and movements (3). Negative symptoms are deficits and functional impairments produced by progression of disease process (4). Clustering of symptoms helps in better understanding and management. Negative symptoms are a frequent and and persistent characteristic of schizoprenia (5).
Cognition is the sum of total mental processes that makes us acquire knowledge and keeps us aware of our surroundings and thus enables us to arrive at appropriate judgments. In simple terms, cognition is thinking and involves acquiring information, processing the acquired information, and arriving at certain conclusions to take action. Cognitive deficits are recognized as enduring and persistent features in schizophrenia and can be neuro-cognitive or relating to social cognition. Neurocognitive deficits are deficits in speed of processing, attention/vigilance, working memory, verbal memory, visual memory, reasoning and problem solving, social cognition.
Broadly, cognition can be divided into 2 broad categories- neurocognition and social cognition. Neurocognition is the process of cognition involving distinct brain areas and particular neural circuits. Social cognition includes those set of cognitive processes involved in interaction with the social world (5). It involves processing information of self and surroundings with respect to social norms. It requires understanding the expression of others and producing responses appropriate to reciprocate. Thus, it forms an essential part for functioning in society appropriately.
Social functioning refers to domains to domains of behavior that involve interactions with others, including social relationships. Social functioning in s c h i z o p h r e n i a i s o p e r a t i o n a l i z e d a t b o t h t h e microcomponent and macrocomponent level. Many of microrcomponents of social functioning are subsumed under rubric of social skills. These typically include the verbal, paralinguistic, and nonverbal components of interpersonal interactions, such as eye contact, facial expression, and latency of speech utterances. A related variable involves social cognition. Many of the core symptoms of schizophrenia, especially those pertaining to cognitive deficits and negative symptoms, are reflected in the poor social skills often shown by persons with the disorder (5). Cognitive functioning is often impaired in schizophrenia and is strongly related to psychological functioning (6).
Over the years, many authors have questioned whether or not schizophrenia is characterized by authentic c o g n i t i v e i m p a i r m e n t . Tr a d i t i o n a l l y, c o g n i t i v e impairment was considered to be significant only in patients with schizophrenia manifest elderly damage. In the past 25 years, evidence has accumulated to challenge this view, but recent studies have clearly demonstrated their presence.
I n a c c o r d a n c e w i t h t h e v i e w t h a t i n schizophrenia any specific deficiencies manifests in cognitive functioning overall. Palmer et al. (7) administered a battery of neuropsychological tests to 171 patients with schizophrenia and compared results with those obtained from 63 healthy subjects. A proportion of 27% of patients with schizophrenia were classified as neuro “normal”. This indicates that cognitive impairment in schizophrenia is significant, in fact is the norm. This study also highlights that the proportion of patients with schizophrenia appear to remain neurological intact. This suggests that the pathophysiology underlying the cognitive deficits often associated with schizophrenia may be distinct from that causing some of the basic clinical characteristics. Evidence supporting this view can also be derived from the study of Goldberg et al. (8), who reported symptomatic improvement after treatment using clozapine, but without accompanying improvement in neuropsychological functioning.
Heinrichs and Zakzanis (9) conducted a comprehensive meta-analysis of cognitiv deficit in schizophrenia, involving comparisons of patients with schizophrenia and control subjects. Most damage was found in the global verbal memory functioning.
Recently, there is a re-occurrence of cognitive factors as indicators critics of schizophrenia and their significance was underlined by several key studies published in the last twenty-five years (10). While the historical position, cognition in schizophrenia increased diminished, is now shown that cognitive impairment is a core area and independently in schizophrenia (11), (12).
Cognitive deficits proved to be very important for several research areas of schizophrenia, such as: u n d e r s t a n d i n g p s y c h o p a t h o l o g y, e p i d e m i o l o g y (indicators of vulnerability), genetics, neuroimaging ( i n c l u d i n g f u n c t i o n a l n e u r o i m a g i n g ) a n d psychopharmacology (these can be used as a parameter of evaluation trials with new therapeutic molecules, or cognitive psychotherapy).
Some areas of cognitive functioning are not affected by schizophrenia.
Current knowledge does not allow an exhaustive listing of cognitive deficits in schizophrenia. A lack of clear understanding of the neural substrates and neuropsychological assessment makes it difficult if problems are cognitive deficits that appear isolated or if they reflect a greater impairment in global domains (13). Cognitive deficits were found consistently in people with schizophrenia in the following areas: memory (immediate and delayed recall, verbal and spatial memory); the attention of (slow cognitive speed); executive functioning (sequencing, organization and flexibility); social functioning. The functions of language, motor and visuospatial found to be less affected consistently in people with schizophrenia.
THE RESEARCH OBIECTIVES
The main objectives of the research were: verify and assess the possibility of positive symptoms, negative and disorganization of patients diagnosed with schizophrenia through PANNS Scale; checking possibility of identifying and assessing the cognitive deficits of patients with a diagnosis of schizophrenia through cognitive tests; assessing cognitive functioning changes in patients with schizophrenia who received treatment with antipsychotic drugs.
METHODOLOGYAND SUBJECTS
To investigate the obiectives we used: Scale for a s s e s s i n g p o s i t i v e s y m p t o m s , n e g a t i v e a n d disorganization (Positive and Negative Syndrome Scale the (PANSS), and a battery of tests, designed to measure some constructs and cognitive functions frequently disturbed in schizophrenia.
Rating Scale clinical symptoms (PANSS scale) was developed in the 1980s by addressing deficiencies in the Brief Psychiatric Rating Scale (BPRS), used to assess positive symptoms (plus) and negative (minus) of schizophrenia and other disorders psychotic. PANSS comprises 30 items differentiated three subscales: seven items covering the positive symptoms (eg hallucinations and delusions), covers seven negative symptoms (eg b l u n t e d a f f e c t ) , 1 6 i t e m s c o v e r i n g g e n e r a l psychopathology (eg, guilt, non-cooperation).
Each item is rated on a Likert type scale with points 1 to 7, according to the presence and severity of symptoms: 1 = absent, 2 = minimal, 3 = easy, 4 = moderate, 5 = moderately severe, 6 = severe, 7 = extremely severe. Each item of the PANSS is accompanied by a complete definition and detailed evaluation criteria for all 7 points of appreciation. Fidelity scales each has been demonstrated, it has a very good internal consistency. Also, the validity of the instrument is very good relationship with measurements based on severity of symptoms. PANSS is a widely used tool to measure severe psychopathology in adult patients with schizophrenia. Scala has become a standard tool for assessing clinical outcomes in treatment studies of schizophrenia and other psychotic disorders and has been shown to be sensitive to treatment change. Scale is often used in research to check drug efficacy.
Cognitive tests used in research were: Verbal memory (MV); Sequence number (SN); Test chips (TJ); Semantic verbal fluency (FV); Coding (substitution) symbols (CS); Tower of London (TL); Test point ( TL).
Cognitive tests provide information on the percentage changes of various quantitative physical activities, such as attention, memory, intelligence, etc. Additional information on the cognitive functions are designed to complement the results of psychiatric and physical examination can provide information on efficacy in improving cognitive deficits specific to patients diagnosed with schizophrenia. Overall, the results obtained through these tests are determined by ensuring the participation and cooperation of patients required tasks. In general, it is estimated that the test results suggest a cognitive impairment fronto-temporal area of the brain.
Subjects were patients admitted and treated initially in the Psychiatric Hospital Al. Obregia and subsequently in ambulatory conditions.
The criteria for inclusion of research subjects were: age (20-55 years); patients diagnosed with schizophrenia (in whatever form) as DSM IV TR(14), criteria and had at least two previous episodes; patients who discontinued antipsychotic medication at least three months before the current episode; patients were able to understand, follow the instructions to achieve the cognitive tests and accept active participation; patients with higher PANSS scale score of 70 points; patients who have significant concomitant somatic disorders in the acute period, but only the control treatment, patients who have addictive substances. Research began with a group of 55 patients diagnosed with schizophrenia, during the research three were excluded the subjects which did not unfulfill conditions for inclusion provided.
RESULTS AND ANALYSIS
In Tables 1, 2 and 3 are the main demographic information included in the research subjects
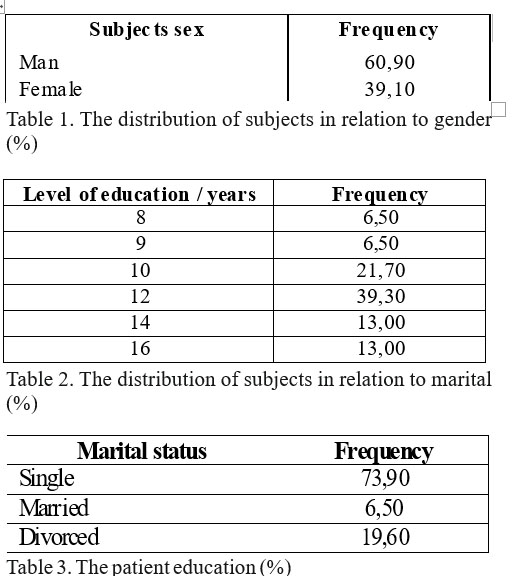
The following are analyzed and interpreted results of PANSS scale and cognitive tests in the two times of measurements: baseline (admission) and final (after a period of one year of treatment).
Statistical analysis of results obtained with methodology was performed using SPSS-18 program. Descriptive statistics were determined, tests of significance of differences between averages scores, the relationship between different values of the variables measured.
Descriptive statistics values of the evaluation results with Scale PANSS subjects are presented in tables
4 and 5, the difference for the two times of measurement.
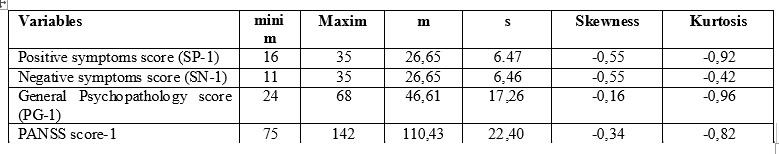
Table 4. The values for the variables descriptive statistics PANSS – initial measurement (1)
The data presented in Table 4 highlights: amplitude, mean, standard deviation scores relatively high for each subscale of PANSS. Symmetry and kurtosis indicators showed values indicating a relatively normal distribution of the results of subjects variables PANSS Scale-1 (see Table 4).
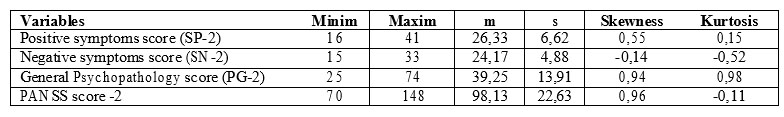
Table 5. Values for the variables descriptive statistics PANSS – final measurement (2)
The data presented in Table 5 highlights: amplitude, mean, standard deviation scores relatively high for each subscale of PANSS. Symmetry and kurtosis indicators showed values indicating a relatively normal distribution of the results of subjects variables PANSS Scale-2 (see Table 5).
To assess the significance of differences between averages scores from the two times of measurement using PANSS Scale there was used t test for dependent samples. The results are presented in Table 6.
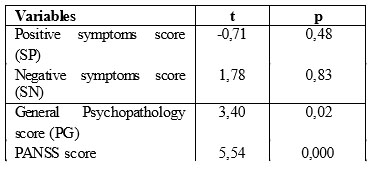
Table 6. The t values of the average test scores significance of the two moments of measurement
The data in Table 6 indicate that there were no significant differences between averages obtained for positive symptoms subscale (t = -0.71, p > 0.05) and negative symptoms subscale (t = 1.78, p > 0. 05).
Significant differences between average scores of the two measurements were recorded for the general psychopathology score (t = 3.40, p < 0.05) and PANSS score (t = 5.54, p < 0.01). These results demonstrate that medical treatment to patients between the two moments of assessment, had a positive effect on symptoms included in the highest subscale score and general psychopathology score included in the PANSS global scale. Also, by overlapping scores, significant differences were obtained between score PANSS-1 and score PANSS-2.
These results are highlighted by the results of analysis of correlation coefficients values of the PANSS subscales scores and PANSS score in both times of assessment (see Table 7).
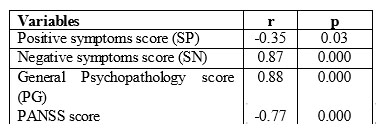
Table 7. The values of correlation coefficients between scores Scale PANSS variables in the two times of measurement
The values of the correlation coefficient between variables included in Table 7 shows the existence of a significant relationship, inverse (r = -0.35, p < 0.05) between positive symptoms scores from the two times of assessment. This relationship indicates that the treatment is significantly reduced positive symptoms in patients investigated event. This type of relationship, but significantly higher intensity is present in the case of global PANSS Scores (r = -0.77, p
< 0.01), indicating that the treatment effect is positive on all symptoms measured by PANSS scale.
The following are analyzed and interpreted the results in cognitive tests in two times of measurements: baseline (admission) and final (after a period of one year of treatment). Descriptive statistics were determined, tests of significance of differences between averages scores, the relationship between different values of the measured variables.
Values of descriptive statistics results of the evaluation subjects with cognitive tests are presented in tables 8 and 9, in a differentiated way to two moments of measurement.
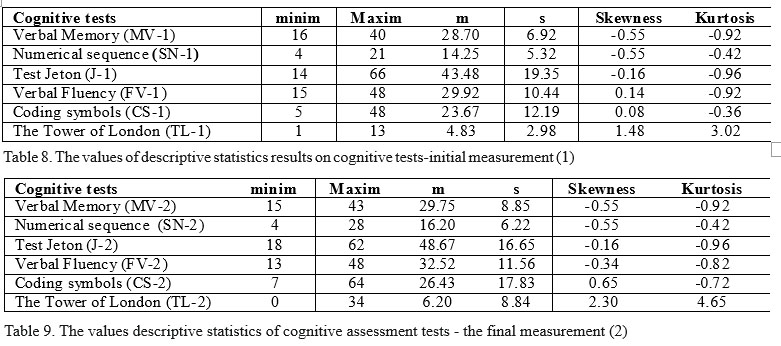
The data presented in Table 8 and 9 are highlights: amplitude, mean, standard deviation scores relatively high for each subscale of PANSS. Symmetry and kurtosis indicators showed values indicating a relatively normal distribution of the results of subjects variables PANSS Scale-2.
To assess the significance of differences between the two averages yields moments of measurement using cognitive tests we used t test for dependent samples. The results are presented in Table 10.
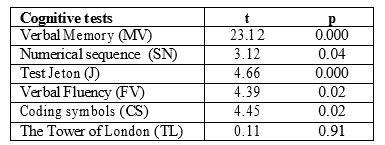
Table 10.The t test values of significance of differences between mean
The data in Table 10 indicate that there were significant differences between subjects environments yields the following cognitive tests: Verbal memory (t =
23.12, p < 0.01), Sequence number (t = 3.12, p < 0.05); Test Chip (t = 4.66, p < 0.01), Verbal fluency (t = 4.39, p
<0.05), Encoding symbols (t = 4.45), p < 0.05). The Tower of London test have not obtained significant differences between subjects in the media yields two moments of measurement (t = 0.11, p > 0.05).
Table 11 presents the correlation coefficients between the values of yields on cognitive tests used and significance of relations in the two times of measurements.
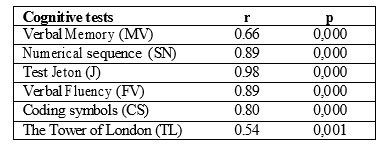
Table 11. The values of correlation coefficients between scores of cognitive evaluation tests
Values yields correlation coefficients of subjects on cognitive tests in the two times of measurement (see Table 11) are highly significant (p < 0.01). The correlation coefficients with the highest values were registered at Chip test (r = 0.98, p < 0.01), Sequence number and Verbal fluency (r = 0.98, p < 0.01), Encoding symbols ( r = 0.80, p
< 0.01). The Verbal memory and cognitive tests Tower of London were obtained correlation coefficients of the lower, r = 0.66, p < 0.01 respectively r = 0.54, p < 0.01.
These highly significant relationships between cognitive test scores in the two times of measurement indicates that the treatment is to maintain a relatively stable level of cognitive performance in patients investigated.
Moreover, these relations show that the samples used for measuring physical characteristics that, while positive values of r indicate a directly proportional relationship: thus an increase in the duration of administration of treatment can lead to improved measured cognitive characteristics.
In Table 12 are values of correlation coefficients between subscales and scales PANSS scores and cognitive tests at initial evaluation.
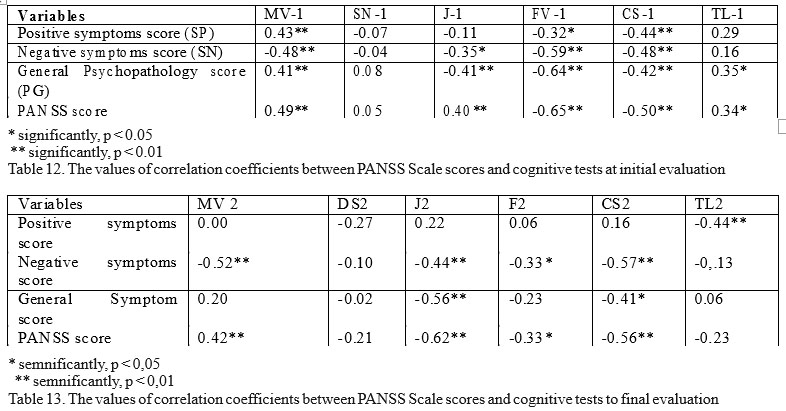
A general observation of the data in Table 13 shows that the levels of correlation coefficients values
between PANSS scores and results of cognitive tests subjects are different from the initial assessment.
Positive symptoms score-2 significantly correlated negatively with performance of subjects Tower of London (r = – 0.44, p < 0.01), demonstrating that cognitive tasks demands deficiencies highlighted by the other samples did not longer show significantly. Thus, correlation coefficients yield positive symptoms Verbal memory tests-2 (r = 0.00, p > 0.05), Verbal fluency-2 (r = 0.06, p >
0.05) and Coding symbols -2 (r = 0.16, p > 0.05) are very low in absolute value and insignificant. In this case, we can say that the treatment significantly influenced the manifestation of positive symptoms of schizophrenia in patients one year after treatment.
Between negative symptoms score-2 and yields the cognitive tests were not made significant changes compared with the initial assessment. There was a significant change in the relationship between negative symptoms and verbal fluency test yield-2 (r = -0.33, p >
0.05). Maintain other relationships relative to the same level as the initial assessment shows that cognitive deficits manifested when negative symptoms are more resistant to change.
If general psychopathological symptom score-2 compared with the initial assessment, record the following situation: low levels of correlation coefficients and statistical significance with verbal memory performance in-2 (r = 0.20, p > 0.05), verbal fluency -2 (r = -0.23, p >
0.05), Tower of London-2 (r = 0.06, p > 0.05), maintaining relatively the same level of correlation coefficients to chips test -2 ( r = – 0.56, p < 0.01), encoding symbols (r = – 0.41, p < 0.05).
If PANSS Score-2 compared with the initial assessment, record the following situation: low levels of correlation coefficients and statistical significance with verbal memory performance in-2 (r = 0.42, p < 0.05), verbal fluency-2 (r = -0.33, p > 0.05), Tower of London-2 (r = -0.23, p > 0.05), maintaining relatively the same level of correlation coefficients to chips test -2 (r = – 0.62, p < 0.01), encoding symbols (r = – 0.56, p < 0.05).
CONCLUSIONS
Schizophrenia is associated over time with a high degree of cognitive disorders and the establishment and maintenance treatment could be associated with an improvement in this function.
The main objectives of the research were checking the possibility of identification and assessment of positive symptoms, negative and disorganization of patients diagnosed with schizophrenia through PANNS Scale, checking identification and assessment of possible c o g n i t i v e d e f i c i t s o f p a t i e n t s d i a g n o s e d w i t h schizophrenia by testing cognitive assessment of changes in cognitive functioning in patients with schizophrenia who received treatment with antipsychotic drugs.
Patients were hospitalized and treated initially in the Psychiatric Hospital Al. Obregia and subsequently in ambulatory conditions. Research began with a group of 55 patients diagnosed with schizophrenia, during the research three were excluded the subjects which did not unfulfill conditions for inclusion provided.
Research results show that medical treatment to patients between the two moments of assessment, had a positive effect on symptoms included in the highest subscale score and general psychopathology scale global PANSS score. Also, by overlapping scores, significant differences were obtained between PANSS score, initial assessment and final assessment. Thus, there were significant differences between the averages scores from the two measurements in general psychopathology subscale score (t = 3.40, p < 0.05) and PANSS global score (t = 5.54, p < 0.01). This difference indicates that the treatment is significantly reduced positive symptoms in patients investigated event.
Statistical analysis found significant differences between subjects environments yields between the two moments of measurement, the following cognitive tests: verbal memory (t = 23.12, p < 0.01), sequence number (t = 3.12, p < 0.05); Chip Test (t = 4.66, p < 0.01), verbal fluency (t = 4.39, p < 0.05), encoding symbols (t = 4.45), p < 0.05). The Tower of London test have not obtained significant differences between subjects in the media yields two moments of measurement (t = 0.11, p > 0.05).
These highly significant differences between cognitive tests scores in the two times of measurement indicates that the treatment is to improve or maintain a relatively stable level of cognitive performance in patients investigated. Based on these data we can state the following: cognitive performance tests provide data highlighted significant diagnosis, clinical evaluation methods and psychoneurological are complementary, each providing information useful for determining proper diagnosis and treatment, efficacy increases by specifying nature deficit and setting off a medical or psychological treatment strategies, the manifestation of symptoms are reduced under the influence of antipsychotic treatment, and severity of symptoms decrease in intensity. Should also be noted that there is a relationship of interdependence between different areas of cognition, they are influencing each other and empowering themselves. Thus, it becomes difficult to distinguish strictly the contribution of a cognitive domain to obtain a certain return, and to clearly differentiate the type of cognitive deficit characteristic of schizophrenia.
The research highlights a number of factors that can influence the evaluation and interpretation of results obtained through the methodology described: the availability and interest for participation in patient assessment of symptoms using PANSS Scale cognitive tests and solving tasks; relatively long time required to use Scale PANSS and cognitive tests solving tasks; methodology used to ensure adequate conditions require evaluation by its subjects; use the methodology requires a relatively high time for both the specialist and the patient; use the methodology requires specialized training.
REFERENCES
1. Prelipceanu D. Psihiatrie-Note de curs. Bucureşti: Ed. Medica, 2003.
2. Harvey PD, Keefe RS. Studies of cognitive change in patients with schizophrenia following novel antipsychotic treatment. Am J Psychiatry 2001;158: 176-84.
3. Berrios GE. Positive and negative symptoms and Jackson: A
conceptual history. Arch Gen Psychiatry 1985;42: 95-7.
4. Pogue-Geile MF, Harrow M. Negative and positive symptoms in schizophrenia and depression: A follow up. Schizophr Bull 1984;10: 371- 87.
5. Lieberman JA, Stroup TS, Perkins OD. Essentials of Schizophrenia. Washington DC, London, 2012.
6. Green MF, Olivier B, Crawley JN, Penn DL, Silverstein S. Social
cognition in schizophrenia: Recommendations from the measurement and treatment research to improve cognition in schizophrenia new approaches conference. Schizophr Bull 2005;3: 882-7.
7. Palmer BW, Heaton RK, Paulsen JS et al. Is it possible to be schizophrenic yet neuropsychologically normal? Neuropsychology 1997;11: 437–446.
8. Golberg TE, Greenberg RD, Griffin SJ et al. The effect of clozapine on cognition and psychiatric symptoms in patients with schizophrenia. British Journal of Psychiatry 1993;162: 43–48.
9. Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: A quantitative review of the evidence. Neuropsychology 1998;12: 426–445.
10. Kraus MS, Keefe RS. Cognition as an outcome in schizophrenia. Br J Psychiatry 2007;50: 46-51.
11. Dias VV, Brissos S, Frey BN, Andreazza AC, Cardoso C, Kapczinski F. Cognitive function and serum levels of brain-derived neurotrophic factor in patients with bipolar disorder. Bipolar Disord 2009;11: 663-71.
12. Saykin AJ, Shtasel DL, Gur RE et al. Neuropsychological deficits in neuroleptic naïve patients with first episode schizophrenia. Archives of
Psychiatry 1994;5: 124–131.
13. Bilder RM, Goodman RS, Robinsons D et al. Neuropsychology of first-episode schizophrenia: initial characterisation and clinical correlates. American Journal of Psychiatry 2000;157: 549–559.
14. DSM-IV-TR. Asociaţia Psihiatrilor Liberi din România. Bucureşti, 2003.
***



