POSTOPERATIVE DELIRIUM INCIDENCE AND OXIDATIVE STRESS IN LAPAROSCOPIC SURGERY
Abstract
Postoperative delirium is a common complication of all types of surgery, especially in elderly patients (2). Overproduction of free oxygen radicals and decrease of organism defense mechanisms is believed to be involved in multiorgan failure, especially in the brain (4). It is important to determinate the susceptibility, incidence and preventive measures for postoperative delirium (8). Our objective was to identify an oxidative stress indicator that predicts the appearance of postoperative delirium in patients that undergoes laparoscopic renal or gynecological surgery for malignant diseases and the possible correlations between certain anesthetic drugs and postoperative delirium occurrence. This study included 29 patients that were treated for localized kidney or uterine cancer by trans peritoneal laparoscopic radical surgery procedures (nephrectomy or hysterectomy) between 2014 and 2016. They were randomized in two groups: the sevoflurane group (n=14 patients) and propofol group (n=15 patients). Blood samples were collected before anesthesia induction, at the end of surgery and at 24 h after surgery and the levels of malondialdehyde (MDA) and superoxide dismutase (SOD) were measured. Postoperative delirium was assessed using Confusion Assessment Method for the ICU (CAM-ICU). All patients with delirium from both groups developed the condition on the first postoperative day. In the sevoflurane group, postoperative delirium has observed in 6/14 patients (42%) and in the propofol group, 5/15 patients (33%) have developed the same postoperative syndrome. There was a significant increase of malondialdehyde levels in the delirium group compared to the non-delirium group in patients, sevoflurane and propofol, at the end of surgery. (p<0.05) There were statistical difference between delirium group and non-delirium group in both sevoflurane and propofol patients, regarding superoxide dismutase levels before anesthesia induction (p<0.05). Postoperative delirium incidence can be predicted by preoperative superoxide dismutase levels assessment in patients that undergoes laparoscopic urologic or gynecological surgery for malignant diseases.
INTRODUCTION
Delirium is a transient mental syndrome of acute onset which is defined by global impairment of cognitive status, a reduced level of consciousness, perceptual and emotional disturbances, impairment of attention, psychomotor activity abnormalities and impairment of sleep, secondary to a general medical condition (1), having a complex multifactorial, and not yet fully understood, etiology.
D e l i r i u m r e p r e s e n t s t h e m o s t c o m m o n psychiatric syndrome which appear in the general hospital setting, affecting between 15% and 60% of medical and surgical inpatients. (2) It is correlated with increased morbidity and mortality, prolonged hospital stays, and decline of cognitive status. (3, 4, 5) The prevalence of delirium in postoperative patients ranges from 10% to 51%. (6) P o s t o p e r a t i v e d e l i r i u m i s a c o m m o n complication of all types of surgery, especially in elderly patients. The incidence of delirium in elderly postoperative patients is 15% to 53% and as high as 80% in elderly patients that require intensive care. (7) One-quarter of delirious elderly patients dies within 6 months. (8)
The cause of the high incidence of postoperative delirium in elderly patients is unclear, but a few mechanisms were proposed. The pathophysiology of delirium is associated with a variety of etiologies: reduced cerebral perfusion/oxygenation (9, 10), imbalance of noradrenergic/cholinergic neurotransmission (11),
imbalance of phenylalanine/tryptophan (12), preoperative cognitive dysfunction, as well as low antioxidant levels. (13)
Increased oxidative activity associated with decreased antioxidative parameters during surgery was proved by various studies. Oxidative stress means an increased formation of free radicals. The most affected organ during the oxidative stress is the cerebral tissue because it has large lipid content, an increased oxidative metabolism and a low antioxidant status. (13) Therefore, the cerebral tissue is highly affected by the increased free oxygen radicals, hydrogen peroxide and superoxide radicals. (14)
The organism tries to protect itself against free oxygen radicals and produces antioxidant enzymes, such as superoxide dismutase (SOD), glutathione peroxidase (GSH) or catalase (CAT), which represent a protective mechanism. (13)
Overproduction of free oxygen radicals and decrease of organism defense mechanisms is believed to be involved in multiorgan failure, especially in the brain. It is important to determinate the susceptibility, incidence and preventive measures for postoperative delirium. It has been confirmed that oxidative stress markers and antioxidative markers can predict postoperative delirium occurrence in cardiopulmonary bypass surgery. (13)
There are only few studies concerning the correlation between oxidative stress, antioxidant activity, anesthetic drugs and postoperative delirium in laparoscopic surgery for urogenital malign pathologies.
The aim of this paper is to identify an oxidative stress indicator that predicts the appearance of postoperative delirium in patients that undergoes laparoscopic renal or gynecological surgery for malignant diseases and the possible correlations between certain anesthetic drugs and postoperative delirium occurrence.
Sevoflurane is a volatile anesthetic drug used in many surgical procedures due to its many beneficial properties. It can be used both in the induction and maintenance of general anesthesia during surgery. Propofol is an intravenous anesthetic with known antioxidant properties that is commonly used for the induction and maintenance of anesthesia during surgery.
MATERIALS AND METHODS
We enrolled in this prospective study a number of 29 patients that were treated for localized kidney or uterine cancer by transperitoneal laparoscopic radical surgery procedures (nephrectomy or hysterectomy) between 2014 and 2016. They were randomized in two groups: the sevoflurane group (n=14 patients) and propofol group (n=15 patients).
All patients enrolled in the study were elderly patients (age above 65 years), with ASA (American Society of Anesthesiology) evaluation I-III and undergoing elective renal or gynecologic laparoscopic surgery for malignant conditions. Exclusion criteria included: a history of propofol or sevoflurane allergy, multiple or severe comorbidities (severe cardiac disease, severe chronic obstructive pulmonary disease, severe hepatic disease or severe renal disease), preexistent cognitive impairment.
The study protocol was conducted in accordance with the Helsinki declaration (2008) and approved by the Ethics Committee of the Emergency Clinical Hospital Craiova. Written informed consent was obtained from each patient.
All patients had general anesthesia. Patients from b o t h g r o u p s w e r e r o u t i n e l y m o n i t o r e d b y e l e c t r o c a r d i o g r a m – D I I d e r i v a t i o n o n E C G , pulsoximetry, capnography, pletismography, blood pressure, and urine output. All patients were pre- medicated 1 h before the surgery with midazolam 0.1 mg/kg.
In the sevoflurane group, patients initially received inhalator sevoflurane for anesthesia induction started at 8% and gradually decreased until sevoflurane MAC (minimum alveolar concentration) reached 2-2.5%. Subsequently remifentanyl 1 µg/Kg over 30-60 seconds and rocuronium bromide 0.5-0.6 mg/kg was administered intravenously. Patients were intubated with 7.5-8 mm cuffed endotracheal tube and ventilated with pressure ventilation mode: tidal volume 6-8 ml/kg, respiratory rate
12-16 breath/minute, fraction of inspired oxygen 1, with the aim to achieve a maximum of 45 mm Hg end-tidal carbon dioxide concentration. Anesthesia was maintained with sevoflurane 1-1.5 (MAC), remifentanyl 0.05-2 µg/Kg/min and rocuronium bromide 0.1-0.2 mg/kg as needed. Fluid replacement was performed with 6-8 ml/kg/h of Ringer lactate solution. Extubation was performed according to Aldrett score. Patients received postoperative analgesia with morphine intravenous 0.1 mg/kg alternated with paracetamol 1g intravenous periodically at 6 hours.
In the propofol group, anesthesia was induced with propofol 2 mg/kg followed by remifentanyl 0.1-2 µg/Kg/min and rocuronium bromide 0.6-0.9 mg/kg. Patients were intubated and ventilated by same protocol described above. Anesthesia was maintained with propofol 0.1-0.2 mg/kg/min, remifentanyl 0.05-2
µg/Kg/min and rocuronium bromide 0.1-0.2 mg/kg as needed. Fluid replacement, extubation and postoperative analgesia were performed similarly to the sevoflurane group. None of patients received anticholinergic drugs at the time of extubation.
Blood samples were obtained from peripheral veins preoperatively before anesthesia induction, at the end of surgery and at 24 hours postoperatively in order to measure the levels of malondialdehyde (MDA). Blood samples were separated by centrifugation at 1200 rpm within 45 min of sampling and stored at −20°C until they were analyzed. Malondialdehyde was measured by high performance liquid chromatography (HPLC) with fluorescence detection. Values were measured as µmol/l of MDA. Blood samples for superoxide dismutase (SOD) measurement were immediately stored at 2-8°C until they were analyzed. SOB was assessed by the photometric technique (enzymatic method). Values were measured as U/g Hb.
Postoperative delirium was assessed using Confusion Assessment Method for the ICU (CAM-ICU) three times per day immediately after surgery. Delirium assessment is a part of the overall consciousness assessment. The consciousness has two parts: level of consciousness and content of consciousness. Initially the level of consciousness was assessed by a validated sedation/level of consciousness scale, such as Richmond Agitation-Sedation Scale (RASS). Subsequently the assessment of the content of consciousness, CAM-ICU Score was performed. Content of consciousness was assessed only if RASS score is -3 to +4.
Mean and standard deviation values were determined for all parameters in the two groups. We usedStudent’s t-test to analyze the differences between variables in the two groups. P-values of 0.05 or less were considered statistically significant. Data was analyzed by MedCalc and SPSS statistical software.
RESULTS
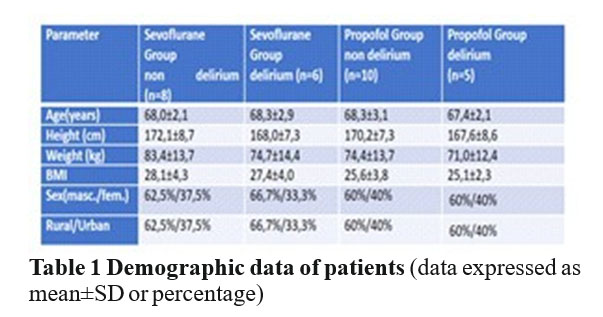
Demographic data for age, height, weight, body mass index (BMI), sex, living area, are shown in Table 1. There were no statistically significant differences between the two groups delirium and non-delirium in both sevoflurane or propofol patients. (p = ns)
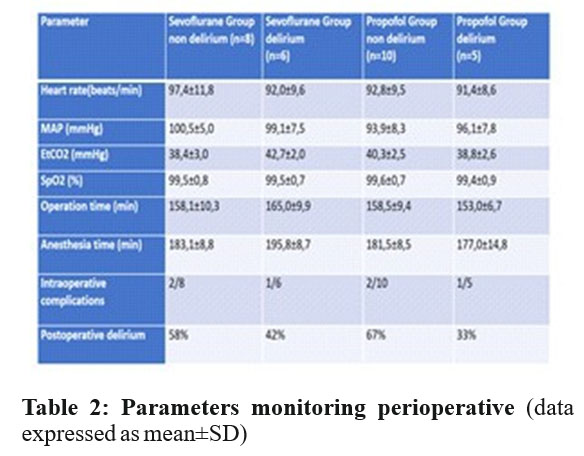
There were no significant differences among the delirium or non-delirium groups in sevoflurane or propofol patients regarding surgery time, heart rate, mean arterial pressure, end-tidal carbon dioxide, peripheral oxygen saturation, duration of anesthesia, and intraoperative complications (p = ns).
All patients with delirium from both groups developed the condition on the first postoperative day. In the sevoflurane group, postoperative delirium has observed in 6/14 patients (42%) and in the propofol group, 5/15 patients (33%) have developed the same postoperative syndrome. (Table 2)
For patients that received volatile anesthetic (sevoflurane) malondialdehyde levels, were significantly increased in both groups, delirium and non-delirium, at the end of surgery (7,3±0,8 µmol/l, respectively 8,1±0,8 µmol/l) compared with those before anesthesia induction (3,3±1,0
µmol/l, respectively 3,0±0,6 µmol/l). Subsequently, malondialdehyde levels decreased gradually but not significant in both groups postoperatively at 24 hours to 6,3±1,1 µmol/l, respectively 6,0±0,5 µmol/l. In the propofol group, malondialdehyde levels in non-delirium group before anesthesia induction were 3,2±0,6 µmol/l and increased to 5,9±0,7 µmol/l at the end of surgery and then decreased significantly to 4,5±0,5 µmol/l at after 24 h o u r s a f t e r s u r g e r y. I n t h e p r o p o f o l g r o u p , malondialdehyde levels in delirium group before anesthesia induction were 3,4±0,5 µmol/l, increased to
6,8±0,6 µmol/l at the end of surgery and then decreased significantly to 5,7±0,8 µmol/l at after 24 hours after surgery. (Table 3)
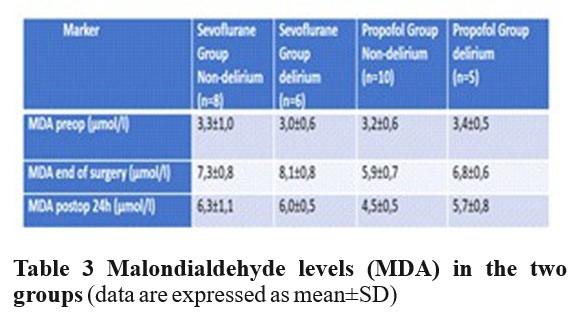
Th er e w er e no s tatis tically s ign ificant differences between the two groups, regarding malondialdehyde levels before anesthesia induction. We recorded a high significant increase of malondialdehyde levels in the sevoflurane group compared to the propofol group, at the end of surgery (p<0.01) and 24 hours postoperatively (p<0.01). There were no statistically significant differences between delirium group and non- delirium group in sevoflurane patients, regarding malondialdehyde levels before anesthesia induction. The same results were in the propofol group. There was significant increase of malondialdehyde levels in the delirium group compared to the non-delirium group in patients, sevoflurane and propofol, at the end of surgery. (p<0.05) We recorded a high statistically significant difference between malondialdehyde levels in the delirium group and non-delirium group in propofol patients at 24 hours postoperative. (p<0.01)
Superoxide dismutase levels in the non-delirium group from the sevoflurane group before anesthesia induction were 2242,1±94,7 U/g Hb. Superoxide dismutase levels in the delirium group from the same sevoflurane group were lower, 2012,7±97,5 U/g Hb. The SOD levels decreased at the end of surgery for both groups, non-delirium and delirium, to 1846,4±64,7 U/g Hb, respectively 1776,5±60,3 U/g Hb, and increased to
2039,4±106,3 U/g Hb, respectively 2062,8±72,9 U/g Hb. Superoxide dismutase levels in the non-delirium group in propofol patients before anesthesia induction were 2170,8±98,4 U/g Hb and significant lower in delirium group from propofol patients, 2004,0±130,0 U/g Hb, decreased slightly at the end of surgery to 2064,4±56,9 U/g Hb, respectively to 1932,0±103,1 U/g Hb. Superoxide dismutase levels increased in the non-delirium group to 2108,8±79,5 U/g Hb and in the delirium group to 2064,6±71,7 U/g Hb postoperatively after 24 hours (Table 4).
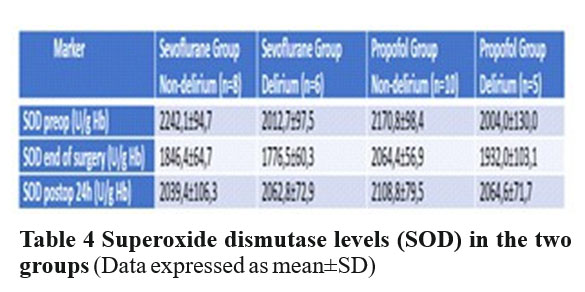
There were no statistical difference between the two groups, sevoflurane and propofol, regarding superoxide dismutase levels before anesthesia induction and at 24 hours after surgery. The results obtained at the end of surgery in the two groups differed high significantly (p<0.01). There was statistical difference between delirium group and non-delirium group in both sevoflurane and propofol patients, regarding the same antioxidant marker before anesthesia induction (p<0.05). We recorded a significant decrease of superoxide dismutase levels in both groups, delirium and non- delirium in all patients at the end of surgery, but there was no statistical difference between the same groups late after surgery.
DISCUSSION
Postoperative delirium has remained an important issue for last years because may cause prolonged hospital stay, postoperative dependence, increased of morbidity and mortality especially of elderly people. Delirium develops over a short period of time (hours to days) after surgery and it is usually reversible. (15)
There are three subtypes of delirium: hyperactive, hypoactive and mixed. Hyperactive delirium is characterized by agitation, patients attempts to remove tubes and lines. Hypoactive delirium is characterized by apathy, lethargy and decreased responsiveness. Mixed delirium is when patients alternate between the two other forms. (15)
The cause of the high incidence of postoperative delirium in elderly patients is unclear, but a few mechanisms were proposed. One proposed mechanisms was imbalance between oxidative stress and antioxidant markers levels. (13)
There are only a few researches about postoperative delirium incidence in laparoscopic urologic and gynecologic surgery.
Laparoscopic urologic and gynecologic surgeries are new techniques used for last decades all over the world for kidney and uterine cancer treatment. The method is preferred compared to the open surgical technique due to its multiple advantages. The major advantage of laparoscopic surgery is less stress than in the open operative techniques (16)
Operative stress is characterized by oxidative stress. (17) Laparoscopic surgical techniques, being less traumatic and less aggressive, are characterized by less severe oxidative stress than the open surgical techniques used in renal or gynecological surgeries. (18, 19)
Oxidative stress is the presence of free oxygen radicals in excess of the buffering capacity of antioxidants. Oxidative stress is an expression of oxidant and antioxidant biomarkers imbalance. (20) Thus, the most correct approach for the determination of oxidative stress is to evaluate and compare the oxidative damage parameter and the antioxidant parameters. (21)
In this paper, we studied malondialdehyde as an oxidative stress marker and superodioxide dismutase as an antioxidant marker, and correlation between that two markers, anesthetic drugs and postoperative delirium in laparoscopic surgery for urogenital malign pathologies. We noticed a lower number of patients with delirium in the propofol group compared to those in the sevoflurane group (33% versus 42%)
Malondialdehyde levels had a significant increase immediately postoperative in the both groups, non- delirium and delirium, in sevoflurane patients, followed by a similar decrease in both groups. Similar results were obtained by Rifat Karlidag et al in their study about predictors of delirium using preoperative oxidative processes in patients undergoing cardiopulmonary bypass surgery, (13)] and Mu-Huo Ji et al in 2013 about the study on 83 patients with orthopedic surgery procedures and early postoperative delirium. (22) We noticed that malondialdehyde levels increases is less significant in the propofol group than in the sevoflurane group at both immediate and late postoperative time points.
Superoxide dismutase levels are decreased preoperatively in all patients that developed delirium in b o t h s e v o f l u r a n e a n d p r o p o f o l g r o u p s , w h i l e postoperative superoxide dismutase levels are significantly decreased in the sevoflurane group and slightly decreased in the propofol group for all patients regardless of delirium development. Superoxide dismutase levels were increased at 24 hours postoperatively in all patient groups.
These findings suggest the involvement of oxidative stress in the postoperative delirium development. Patients with postoperatory delirium had lower antioxidant protection. The results confirm the known antioxidant role of propofol. Our data is in line with the study of Konstantinos Kalimeris et al. from 2013 that studied the antioxidative role of propofol vs. sevoflurane upon the postoperative d e l i r i u m o c c u r r e n c e i n p a t e n t s w i t h c a r o t i d endarterecomy. (23)
The risk of postoperatory delirium occurrence may therefore be evaluated by preoperative superoxide dismutase value. The patients with increased risk for this syndrome could subsequently avoid it by receiving postoperative prophylactic low doses of haloperidol that is the standard treatment of postoperatory delirium. Furthermore, patients with high risk for postoperatory delirium may receive before surgery antioxidant agents to protect them against this syndrome.
CONCLUSION
Significant oxidative stress and antioxidant activity is proved by the increased malondialdehyde and d ec r e a s ed s u p er o x i d e d is m u tas e l e v e l s d u r i n g laparoscopic surgery for malignant urologic and gynecologic conditions. Perioperative oxidative stress is significantly decreased by propofol used in general anesthesia due to its antioxidant proprieties. Postoperative delirium incidence can be predicted by preoperative superoxide dismutase levels assessment.
CONFLICT OF INTERESTS
Authors have no conflict of interests to declare.
REFERENCES
1.Diagnostic and Statistical Manual of Mental Disorders. DSM-IV-TR, Fourth Edition, Text Revision, 2000.
2.Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: an underrecognized syndrome of organ dysfunction. Semin Resp Crit Care Med 2001; 22:115–126.
3.McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med 2002; 162:457–463.
4.McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc 2004; 51:1539–1546.
5.McCusker J, Cole M, Dendukuri N, Belzile E, Primeau F. Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ 2001; 165:575–583.
6.Wise MG, Hilty DM, Cerda GM, Trzepacz PT. Delirium (confusional states), in Textbook of Consultation-Liaison Psychiatry: Psychiatry in the Medically Ill. Edited by Wise MG, Rundell JR. Washington, DC, American Psychiatric Publishing, Inc, 2002, 257–272.
7.Demeure MJ, Fain MJ. The elderly surgical patient and postoperative delirium. J Am Coll Surg 2006; 203:752–757.
8.Fann JR. The epidemiology of delirium: a review of studies and methodological issues. Semin Clin Neuropsychiatry 2000; 5:64–74.
9.Nollert G, Mohnle P, Tassani-Prell P, et al. Postoperative neuropsychological dysfunction and cerebral oxygenation during cardiac surgery. Thorac Cardiovasc Surg 1995; 43:260 – 4.
10.Gokgoz L, Gunaydin S, Sinci V, et al. Psychiatric complications of cardiac surgery postoperative delirium syndrome. Scand Cardiovasc J 1997; 31:217 – 22.
11.Eikelenboom P, Hoogendijk WJG. Do delirium and Alzheimer’s dementia share specific pathogenetic mechanisms? Dement Geriatr Cogn Disord 1999; 10:319 – 24.
12.van der Mast RC, van den Broek WW, Fekkes D, Pepplinkhuizen L, Habbema JD. Is delirium after cardiac surgery related to plasma amino acids and physical condition? J Neuropsychiatry Clin Neurosci 2000; 12:57 – 63.
13.Karlidag R., Unal S., Ozlem H., Karabulut AB, Battalog˘lu, BY., But A., Ozcan C. The role of oxidative stress in postoperative delirium. General Hospital Psychiatry 2006; 28: 418 – 423.
14.Choi BH. Oxygen, antioxidants and brain dysfunction. Yonsei Med J 1993; 34:1 – 10.
15.Association AP. Diagnostic and Statistical Manual of Mental Disorders: DSM 5. Books4US; 2013.
16.Zhang GL, Liu GB, Huang QL, Xing FQ. Comparative study of the impacts of laparoscopic and open laparatomic surgeries on oxidative stress in patients with uterine myoma. Di Yi Jun Yi Da Xue Xue Bao 2004; 24: 907-9.
17.Vanlersberghe C, Camu F Propofol. Handb Exp Pharmacol 2008; 182: 227-252.
18.Allaouchiche B, Debon R, Goudable J, et al Oxidative stress status during exposure to propofol, sevoflurane and desflurane. Anesth Analg 2001; 93: 981-985.
19.Takizawa D, Nishikawa K, Sato E, et al. A dopamine infusion decrease propofol concentration during epidural blockade under general anesthesia. Can J Anaesth 2005; 52: 463-466.
20.Rabus M., Demirbag R., Sezen Y. et al. Plasma and tissue oxidative stress index in patients with rheumatic and degenerative heart valve disease. Turk Kardiyoloji Dernegi Arsivi, 2008; 36 (8): 536–540.
21.Türker SF., DoLan A., Ozan G., KJbar KG, ErJGJr M. Change in Free Radical and Antioxidant Enzyme Levels in the Patients Undergoing Open Heart Surgery with Cardiopulmonary Bypass. Oxidative Medicine and Cellular Longevity 2016, ID 1783728, 5.
22.Mu-Huo Ji, Hong-Mei Yuan, Guang-Fen Zhang, Xiao-Min Li, Lin Dong, Wei-Yan Li, Zhi-Qiang Zhou, Jian-Jun Yang Changes in plasma and cerebrospinal fluid biomarkers in aged patients with early postoperative cognitive dysfunction following total hip-replacement surgery J Anesth 2013; 27:236–242.
23.Kalimeris K., Kouni S., Kostopanagiotou G., Nomikos T, Fragopoulou E., Kakisis J, Vasdekis S, Matsota P, Pandazi A. Cognitive Function and Oxidative Stress After Carotid Endarterectomy: Comparison of Propofol to Sevoflurane. Anesthesia Journal of cardiothoracic and vascular anesthesia, 2013; 27, 6: 1246–1252.
***




