COMORBIDITIES OF ALCOHOL USE DISORDER
Abstract
Introduction: Dual diagnosis is frequent among psychiatric patients. Alcohol use disorder (AUD) negatively affects the treatment and the progression of co- occurring disorders. The reverse could also be valid, other symptoms of other diseases and therapies may hinder the achievement and maintenance of abstinence. Aim: The aim of the present study is to assess the frequency of psychiatric and medical comorbidities, of the prescribed drugs and the hospital costs related to AUD. Methods: Using AtlasMed database, we searched the patients admitted to the Cluj County Emergency Hospital County Emergency Hospital Psychiatry Department, during a one year span, mostly men, accounting for 23% of the total number of hospitalisations and 12.1% of the h o s p i t a l c o s t s . T h e m o s t f re q u e n t p s y c h i a t r i c comorbidities were personality disorders, major depressive disorder (MDD), neurocognitive disorders, alcohol-related psychosis and suicide attempts. The most common medical conditions in alcoholics were alcoholic l i v e r d i s e a s e ( A L D ) , c a rd i o v a s c u l a r d i s e a s e , dyslipidemia, alcoholic polyneuropathy, alcoholic pancreatitis, type 2 diabetes and head injuries. The most commonly prescribed psychiatric medications were Psychiatry Department between January the 1st and benzodiazepines, anticonvulsants and tiapride. December 31st 2016, with a main or secondary diagnosis of alcohol dependence. The socio-demographic (age, gender, geographic area), the psychiatric and medical diagnosis and the prescribed psychotropic medications were recorded. Results: 623 alcoholic patients were admitted to the Cluj Conclusions: Alcohol dependence has become an increasingly stringent public health problem, from the point of view of prevalence, frequent admittances, relapses and comorbidities.
INTRODUCTION
According to the International Classification of Diseases,
10th Revision (ICD-10), alcohol abuse was associated with over 200 medical conditions (1). The presence of alcohol dependence affects the prognosis and treatment of associated diseases, and in the long run increases hospital morbidity and mortality (2). The economic impact is significant, literature studies indicating a 50% increase in costs related to treatment and decreased productivity over abstinent patients (3), with substantially higher indirect costs (4).
Approximately half of alcoholics also have a diagnosis of personality disorder, involving frequent heavy drinking patterns, but not necessarily a worse prognosis if the patients are compliant later on (5).
Depression constitutes a frequent comorbidity, or it can be only part of the alcohol withdrawal syndrome, the later one resolving spontaneously in a few weeks. In addition to the common genetic interface, there is also a neuroimmune hypothesis, both being caused by central nervous system (CNS) inflammation, which provides another potential explanation for this recurrent dual diagnosis (6). Although the literature reports a high prevalence of anxiety disorder among alcoholics (up to 35%), it is difficult to discern if these symptoms are part of alcohol intoxication or withdrawal or make up for a separate diagnosis. An AUD in a psychotic patient increases the risk of relapse and mortality (7). Alcohol induced neuronal destruction generates a spectrum of neuropsychiatric conditions i n c l u d i n g m i l d c o g n i t i v e i m p a i r m e n t ( M C I ) , Wernicke–Korsakoff syndrome (WKS) and dementia (8). Although moderate alcohol intake may decrease the risk of progression from MCI to dementia, heavy drinking has the opposite effect (9).
MATERIALAND METHODS
Using the AtlasMed database, officially employed by the Cluj County Emergency Hospital Psychiatry Department, admissions between January 1st and December 31st 2016 of patients, with a main or secondary diagnosis of alcohol dependence, according to ICD-10 diagnostic criteria were analyzed. Socio-demographic data (age, gender, geographic area), the psychiatric and medical diagnosis and the prescribed psychotropic medications were prescribed. The Analysis ToolPak in Microsoft Office Excel 2010 was used for statistical data analysis and the assessment of relative risk (RR). The study procedures respect confidentiality and are in accordance to the norms of research and were approved by the Local Ethical Committee.
RESULTS
Between January 1st and December 31st 2016, 623 patients were admitted 817 times with a main or secondary diagnosis of alcohol dependence, accounting for 23.02% of the total 3549 hospital admissions. During that one year period, the number of admissions varied between 1 (75.76%) and 9 (one case). Men were over-represented (87%), the mean age was 52.4 years, less for women (50.4 years). Both men and women came mainly from urban areas (64%).
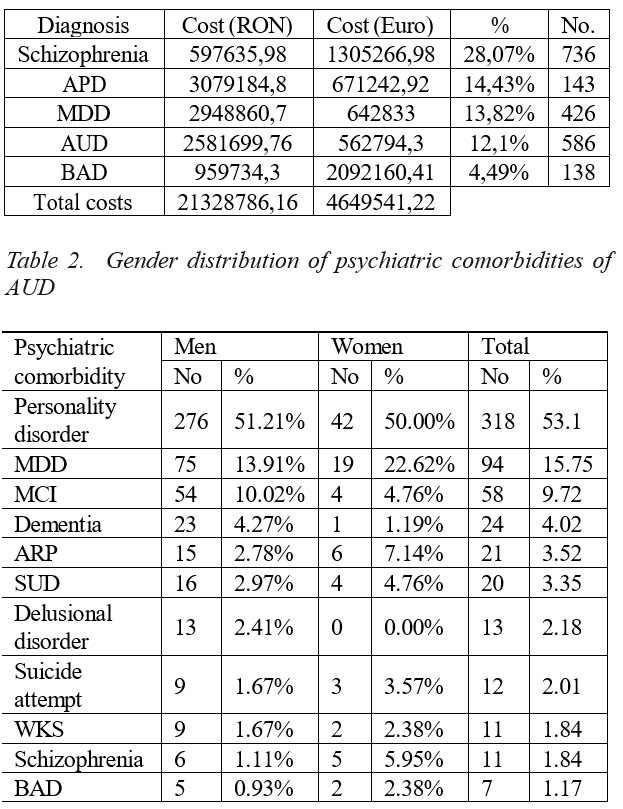
2016 direct hospital costs for AUDs (intoxication, abuse, dependence, withdrawal) were 562794.3 Euro (12.1% of the total costs, placing this disorder on the 4th place on the yearly hospital costs hierarchy according to the main psychiatric diagnosis) (Table 1).
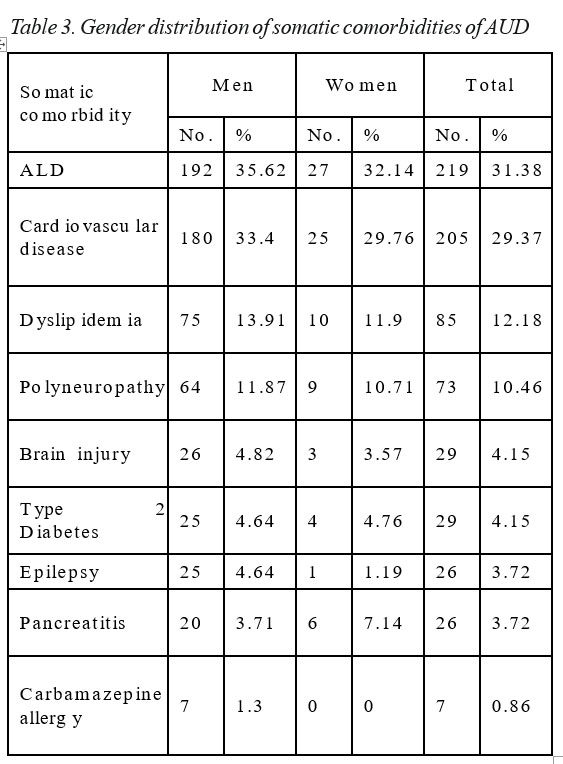
The most common psychiatric comorbidities were personality disorders (53.1%), MDD (15.75%) and neurocognitive disorders (MCI, 9.72%; dementias, 4.02% and WKS, 1.94%) (Table 2). The most frequent personality disorders were emotionally unstable personality disorder, impulsive type, both in men and women, and antisocial personality disorder.
77.52% of the patients were hospitalized for alcohol withdrawal syndrome, the rest of 22.48% were abstinent and were admitted for other disorders. Most often, the subjects experimented an uncomplicated alcohol withdrawal (71.01%), the rest underwent complicated alcohol withdrawal, with seizures (14.07%), with delirium (10.97%) or both (3.93%).
Table 3 shows the distribution of somatic comorbidities of AUD according to gender. 31.14% developed alcohol liver disease (ALD) (men slightly more frequent than women, 35.62% vs 32.14%). 29.37% had a history of cardiovascular disease (hypertension, coronary heart disease, arrhythmias or stroke) and 12.18% had dyslipidemia. The neurological comorbidities were represented by alcoholic polyneuropathy (10.46%), head injuries (5.15%) and epilepsy (3.72%). Type 2 Diabetes is present in 4.15% of patients in both male and female alike.
3.72% developed various stages of alcoholic pancreatitis. Although not a comorbidity per se, carbamazepine allergic reaction was a complication present in 0.86% of the subjects.
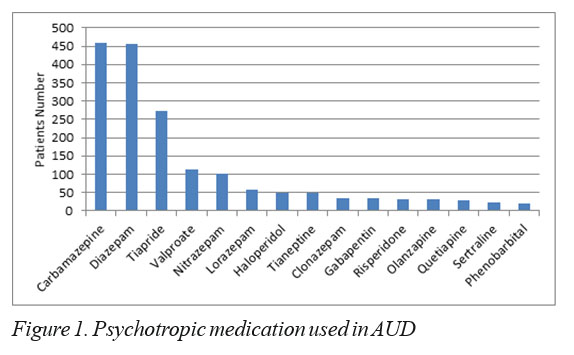
The prescribing trends in psychotropic medications are shown in Figure 1. All the patients received benzodiazepines. Among them, the most prescribed were diazepam (73.19%), nitrazepam (16.05%) and lorazepam (9.31%). For the entire study, the most prescribed drug was carmbamazepine (73.84%). Other prescribed anticonvulsants were valproate (17.98%), gabapentine (5.46%) and phenobarbital (3.37%).
The anticraving medications recommended for the treatment of alcoholism were seldom prescribed. Only 3.85% of the patients admitted in 2016 received opioid antagonists (nalmefene 1.93%, naltrexone 0.64%), aversion therapy with disulfiram (0.96%) or acamprosate (0.32%). It is worth mentioning the use of metronidazole as an antidipsotropic in 1.44% of the patients.
The most prescribed antidepressants for the treatment of the depressed alcoholic patients were tianeptine (41.03%), sertraline (18.8%) and mirtazapine (11.97%). Doxepin (5.13%), trazodone (4.27%), escitalopram (4.27%) and agomelatine (1.71%) were recommended less often.
Excluding tiapride, the third most prescribed drug in the present study (43.98%), typical antipsychotics were given in 11.4% of cases and the atypical ones in 16.37%.
DISCUTIONS
Despite the fact that in the Western countries the gender gap regarding alcohol use is progressively diminishing (10), the Transylvanian population does not follow the same trend. There is still a significant difference between men and women, probably due to the traditional social acceptability of alcohol intoxication in males.
The direct hospital costs of AUD in 2016 places alcoholism on 4th place (12.1%), close to 2nd (acute psychotic disorder, 14.43%) and 3rd place (MDD, 13.82%) but very far from 5th place (bipolar affective disorder, one of the most severe psychiatric disorders, that involves more expensive drugs than the ones usually used for alcoholic patients) (Table 1). For technical reasons, to avoid overlapping reported expenses, these results do not include the costs of admissions with only a secondary diagnosis of AUD. Thus, the real total hospital costs for alcoholics are higher, transforming this addiction into an important public health problem.
Women appeared to be more vulnerable to the complications of heavy drinking. They had a 2.5 times greater risk to develop an alcohol-related psychosis (p=0.044), a 1.62 times higher risk to have comorbid depression and were more predisposed to attempt suicide (3.57% of females vs 1.67% of males). In addition, women had a 3.52 times greater risk to experiment a complicated withdrawal (p=0.0001) and WKS and more female schizophrenic abused alcohol (5.95%) then males (1.11%). MCI and dementias were an exception, since they were almost two times more frequent in men. Anxiety disorders were unexpectedly rarely coded (0.67%), probably through overlapping symptoms of alcohol withdrawal. Patients with a personality disorder had a 1.61 times greater risk to be admitted more than 2 times in one year (p=0.001). Though the gender distribution of emotionally unstable personality disorder, impulsive type was similar, in our study, the borderline type was reported only in females.
As expected, approximately one third of the patients developed alcoholic liver disease, males (36.62%) slightly more than women (32.14%). A similar distribution was reported for cardiovascular diseases, with a mild masculine predominance (33.4% of male vs
29.76% of females). While dyslipidemia was recorded only in 12.18% of the subjects, the real prevalence is probably much higher. By virtue of our study design, dyslipidemia as well as important comorbidities, such as smoking and obesity, could not be assessed, since they are rarely coded as official diagnosis. Thus, a thorough evaluation of the patients’ charts is needed. Alcoholic pancreatitis was less common (3.72%), women were twice as likely to develop significant elevations of serum lipase than men (7.14% of females vs 3.71% of males). Type 2 Diabetes was present in 4.15% of alcoholics, with an equal gender distribution and there were not any patients with type 1 diabetes. Apart from cognitive impairments, alcohol induced neurological complications were polyneuropathy (10.46% of individuals, with similar gender distribution) and head injuries, generally caused by falling during intoxications or during complicated withdrawal seizures (slightly more frequent in men, 4.82% than in women, 3.57%). 3.72% of alcohol dependent individuals had a diagnosis of epilepsy, twice as common in men. Of them, only 23% presented with a complicated withdrawal with seizures, since they were probably covered by their chronic anticonvulsant treatment. Actually a rare complication (only 7 cases or 0.87% of patients, exclusively male), carbamazepine allergic reaction is of major importance since it is potentially lethal. Additionally, since carbamazepine was the most prescribed drug in our study, vigilance is required to catch early signs of anaphylaxis.
Considering that most of the subjects in the present study were admitted for alcohol withdrawal, concurrently to international guidelines, the most prescribed drug classes were benzodiazepines and anticonvulsants. All the patients were treated most frequently with diazepam (73.19%), the main substitution medication for alcohol withdrawal, followed by nitrazepam (16.05%, with insomnia being one of the most distressing symptoms for psychiatric patients) and lorazepam (9.31%). The latter is the drug of choice for elderly and liver impaired patients (in our study, in subjects with alcohol liver disease, lorazepam prescription rose from 8.67% to 12.66%). In these particular situations, diazepam has a higher risk of excessive sedation and respiratory depression (11). Another widely used class was anticonvulsants. As stated earlier, carbamazepine was the most prescribed drug for alcoholic patients in 2016 in our clinic. It was recommended in the short term for preventing seizures (by increasing the convulsant threshold), although some systematic reviews declared it even more effective and with fewer side effects for treating alcohol withdrawal than benzodiazepines (12). In the long term, carbamazepine produces a decrease in drinks per drinking day and a delay in time to relapse (13). In addition to its antiepileptic and mood stabilizing effects on highly impulsive individuals, valproate has the benefits of diminishing heavy drinking days in bipolar patients with a dual diagnosis (14). Seldom prescribed, gabapentin seems to be as efficient as lorazepam in the treatment of mild withdrawal, in outpatients (15), and also, in the long run it prevents craving and relapse (16). Granting that barbiturates are not first-line therapy, in selected cases, phenobarbital proved beneficial for severe complicated withdrawal (in this study, 25.93% of patients with complicated withdrawal with seizures and 5.66% of the ones with delirium received phenobarbital, vs 2.92% of the cases with uncomplicated withdrawal) (17). In the present study, levetiracetam was a preexisting treatment of epileptic patients and was not prescribed for psychiatric purposes. Nevertheless, levetiracetam does not seem to be a suitable choice for alcoholic epileptic individuals, since it is the only anticonvulsant that does not prolong the duration of abstinence and does not decrease heavy drinking (18). In such a situation, considering that ethanol can increase the likelihood of seizures, a tight collaboration with a neurologist could improve the prognosis.
The anticraving medications were seldom prescribed, due to the prohibitive cost of opioid antagonists and acamprosate (which is no longer even available in Romania). The latter and naltrexone are only moderately effective, but significantly reduces the risk of relapse after abstinence is obtained, with minimal side effects (19, 20). Nalmefene, with the advantage of “as needed” administration, seems to be superior to naltrexone, according to some studies (21) (others suggest only a limited efficacy for certain patients (22). Although their effectiveness has yet to be established due to great variability of studies’ design, their use could prove salutary in lack of other viable therapeutic alternatives.
Disulfiram, the only pharmacotherapeutical option for alcoholism for decades, has become a second-line drug because of its potentially dangerous aversive reaction. Nonetheless, its administration under supervision can be useful when other options have failed (adjunct to cognitive-behavioural, educational and psychosocial interventions) (23). There is also the practice of using metronidazole for its alleged aversive properties (1.44% of the patients), yet the evidence of its disulfiram-like reaction in combination with ethanol is scarce (24). Furthermore, a treatment longer than 2 weeks with metronidazole dramatically pauperizes the variability of microbiota, with unforeseeable effects on the functioning of the entire body (25).
Tianeptine was the most widely prescribed antidepressant in the present study, with the advantage that dose reduction is not necessary for liver impaired patients, with or without cirrhosis. Its effectiveness in depressed alcoholics, while delayed to 4 to 8 weeks, was established, however its influence on craving, maintaining abstinence and long term prognosis of alcohol dependence is not clear (26). Lately, tianeptine’s μ opioid receptor agonist activity was proved (27), accountable, apart from the antidepressant and anxiolytic effects (28), for its addictive potential (especially for patients under 50 years, with a history of drug or alcohol abuse) (29). The use of selective serotonin reuptake inhibitors (SSRI) is controversial, since they could trigger heavy drinking, especially for type B alcoholism (earlier onset, more alcohol intake) (30). Furthermore, a series of 93 cases describes even the onset of alcohol dependence after therapy with SSRIs for MDD (31). Still, a safer alternative could be naltrexone in combination with sertraline (but not escitalopram), with positive effects on this dual diagnosis (32). Although doxepin has an indication for depression during alcohol abstinence, in the present study it was rarely used. Because of multiple side effects, it remains a second-line medication. Also, mirtazapine was seldom prescribed, although it is effective in the long term both as an antidepressant, as well as for lowering alcohol consumption (even if other studies suggest that it does not influence alcohol intake, mirtazapine is considered safe for this group of patients) (33, 34). Since it is insufficiently studied in depressed alcoholics, trazodone was prescribed particularly for persistent insomnia after achieving abstinence, notably because it does not appear to influence relapse rates (35).
Antipsychotics were prescribed mostly for psychosis and aggressiveness. A meta-analysis of 13 randomized double blind placebo controlled studies (3 papers on tiapride) did not show any benefit regarding abstinence, craving control or the reduction of the consumed amount of alcohol for neither antipsychotic (36). Tiapride (the third most prescribed drug in our study, 48.98%) is worth special mention. It was prescribed for short term control of agitation and aggressiveness. In the long term, its benefit is controversial, a randomized double blind placebo controlled study noticed earlier and higher rates of relapse for patients that received tiapride (37).
CONCLUSIONS
Alcohol dependence represents a costly public health problem. On the Psychiatry ward in Cluj-Napoca, an alcoholic patient has the following profile, according to our study: an approximately 50 year old man, from an urban area, with at least one psychiatric or somatic comorbidity, admitted for alcohol withdrawal syndrome. More often, men tend to develop a somatic complication and women a psychiatric comorbidity. Cluster B personality disorders were the most frequent in alcoholics. T h e m o s t p r e s c r i b e d c l a s s e s o f d r u g s w e r e benzodiazepines and anticonvulsants, while anticraving medication was rarely recommended.
ABREVIATIONS
ALD – Alcoholic liver disease APD – Acute psychotic disorder ARP – Alcohol-related psychosis AUD – Alcohol use disorder BAD – Bipolar affective disorder CNS – Central nervous system
ICD-10 – International Classification of Diseases, 10th Revision
MCI – Mild cognitive impairment
MDD – Major depressive disorder
SSRI – Selective serotonin reuptake inhibitors
SUD – Substance use disorder (other than alcohol)
WKS – Wernicke–Korsakoff syndrome
TABELS AND FIGURES
Table 1. Annual hospital costs according to the main psychiatric diagnosis
REFERENCES
1.Rehm J, Shield KD. Global alcohol-attributable deaths from cancer, liver cirrhosis, and injury in 2010. Alcohol Res. 2013;35(2):174-83.
2.Schoepf D, Heun R. Alcohol dependence and physical comorbidity: Increased prevalence but reduced relevance of individual comorbidities for hospital-based mortality during a 12.5-year observation period in general hospital admissions in urban North-West England. Eur. Psychiatry. 2015;30(4):459-68.
3.Manthey J, Laramee P, Parrott S, Rehm J. Economic burden associated with alcohol dependence in a German primary care sample: a bottom-up study. BMC public health. 2016;16:906.
4.Laramee P, Kusel J, Leonard S, Aubin HJ, Francois C, Daeppen JB. The economic burden of alcohol dependence in Europe. Alcohol Alcohol.. 2013;48(3):259-69.
5.Newton-Howes GM, Foulds JA, Guy NH, Boden JM, Mulder RT. Personality disorder and alcohol treatment outcome: systematic review and meta-analysis. Br J Psychiatry. 2017;211(1):22-30.
6.Neupane SP. Neuroimmune Interface in the Comorbidity between Alcohol Use Disorder and Major Depression. Front Immunol. 2016;7:655.
7.EMCDDA. Comorbidity of Substance Use and Mental Disorders in Europe: A Review of the Data. EMCDDA Papers. Luxembourg:Publications Office of the European Union; (2015). Available from: http://www.emcdda.europa.eu/publications/insights/comorbidity- substance-use-mental-disorders-europe
8.Hayes V, Demirkol A, Ridley N, Withall A, Draper B. Alcohol-related cognitive impairment: current trends and future perspectives. Neurodegener Dis Manag. 2016;6(6):509-23.
9.Xu G, Liu X, Yin Q, Zhu W, Zhang R, Fan X. Alcohol consumption and transition of mild cognitive impairment to dementia. Psychiatry Clin. Neurosci. 2009;63(1):43-9.
10.Hasin DS, Grant BF. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: review and summary of findings. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1609-40.
11.Soyka M, Kranzler HR, Hesselbrock V, Kasper S, Mutschler J, Moller HJ. Guidelines for biological treatment of substance use and related disorders, part 1: Alcoholism, first revision. World J Biol Psychiatry.
2017;18(2):86-119.
12.Minozzi S, Amato L, Vecchi S, Davoli M. Anticonvulsants for alcohol withdrawal. Cochrane Database Syst Rev. 2010(3):Cd005064.
13.Malcolm R, Myrick H, Roberts J, Wang W, Anton RF, Ballenger JC. The effects of carbamazepine and lorazepam on single versus multiple previous alcohol withdrawals in an outpatient randomized trial. J Gen Intern Med. 2002;17(5):349-55.
14.Salloum IM, Cornelius JR, Daley DC, Kirisci L, Himmelhoch JM, Thase ME. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005;62(1):37-45.
15.Leung JG, Hall-Flavin D, Nelson S, Schmidt KA, Schak KM.The role of gabapentin in the management of alcohol withdrawal and dependence.
Ann Pharmacother. 2015;49(8):897-906.
16.Mason BJ, Quello S, Goodell V, Shadan F, Kyle M, Begovic A. Gabapentin treatment for alcohol dependence: a randomized clinical trial.
JAMA Intern Med. 2014;174(1):70-7.
17.Mo Y, Thomas MC, Karras GE, Jr. Barbiturates for the treatment of alcohol withdrawal syndrome:
A systematic review of clinical trials. J Crit Care. 2016;32:101-7.
18.Richter C, Effenberger S, Bschor T, Bonnet U, Haasen C, Preuss UW, et al. Efficacy and safety of levetiracetam for the prevention of alcohol relapse in recently detoxified alcohol-dependent patients: a randomized trial. J Clin Psychopharmacol. 2012;32(4):558-62.
19.Rosner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M. Acamprosate for alcohol dependence. Cochrane Database Syst Rev. 2010(9):Cd004332.
20.Donoghue K, Elzerbi C, Saunders R, Whittington C, Pilling S, Drummond C. The efficacy of acamprosate and naltrexone in the treatment of alcohol dependence, Europe versus the rest of the world: a meta-analysis. Addiction. 2015;110(6):920-30.
21.Soyka M, Friede M, Schnitker J. Comparing Nalmefene and Naltrexone in Alcohol Dependence: Are there any Differences? Results from an Indirect Meta-Analysis.Pharmacopsychiatry. 2016;49(2):66-75.
22.Palpacuer C, Laviolle B, Boussageon R, Reymann JM, Bellissant E, Naudet F. Risks and Benefits of Nalmefene in the Treatment of Adult Alcohol Dependence: A Systematic Literature Review and Meta- Analysis of 11Published and Unpublished Double-Blind Randomized Controlled Trials. PLoS Med. 2015;12(12):e1001924.
23.Brewer C, Streel E, Skinner M. Supervised Disulfiram’s Superior Effectiveness in Alcoholism Treatment: Ethical, Methodological, and Psychological Aspects. Alcohol Alcohol.. 2017;52(2):213-9.
24.Visapaa JP, Tillonen JS, Kaihovaara PS, Salaspuro MP. Lack of disulfiram-like reaction with metronidazole and ethanol. Ann Pharmacother. 2002;36(6):971-4.
25.Becker E, Schmidt TSB, Bengs S, Poveda L, Opitz L, Atrott K, et al. Effects of oral antibiotics and isotretinoin on the murine gut microbiota. Int. J. Antimicrob. Agents. 2017;50(3):342-51.
26.Favre JD, Guelfi-Sozzi C, Delalleau B, Loo H. Tianeptine and alcohol dependence. Eur Neuropsychopharmacol. 1997;7Suppl 3:S347-51.
27.Gassaway MM, Rives ML, Kruegel AC, Javitch JA, Sames D. The atypical antidepressant and neurorestorative agent tianeptine is a mu- opioid receptor agonist. Transl Psychiatry. 2014;4:e411.
28.Samuels BA, Nautiyal KM, Kruegel AC, Levinstein MR, Magalong VM, Gassaway MM, et al. The Behavioral Effects of the Antidepressant T i a n e p t i n e R e q u i r e t h e M u – O p i o i d R e c e p t o r . Neuropsychopharmacology. 2017;42(10):2052-63.
29.Rouby F, Pradel V, Frauger E, Pauly V, Natali F, Reggio P, et al. Assessment of abuse of tianeptine from a reimbursement database using
‘doctor-shopping’ as an indicator. Fundam Clin Pharmacol. 2012;26(2):286-94
30.Atigari OV, Kelly AM, Jabeen Q, Healy D. New onset alcohol dependence linked to treatment with selective serotonin reuptake inhibitors.
Int J Risk Saf Med. 2013;25(2):105-9.
31.Brookwell L, Hogan C, Healy D, Mangin D. Ninety-three cases of alcohol dependence following SSRI treatment. Int J Risk Saf Med. 2014;26(2):99-107.
32.Pettinati HM, Oslin DW, Kampman KM, Dundon WD, Xie H, Gallis TL, et al. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry. 2010;167(6):668-75.
33.Cornelius JR, Douaihy AB, Clark DB, Daley DC, Chung TA, Wesesky MA, et al. Mirtazapine in Comorbid Major Depression and Alcohol Use Disorder: A Long-Term Follow-Up Study. J Addict Behav Ther Rehabil. 2013;3(1).
34.Cornelius JR, Chung T, Douaihy AB, Kirisci L, Glance J, Kmiec J, et al. Mirtazapine in comorbid major depression and an alcohol use disorder: A double-blind placebo-controlled pilot trial. Psychiatry Res. 2016;242:326-30.
35.Kolla BP, Schneekloth TD, Biernacka JM, Frye MA, Mansukhani MP, Hall-Flavin DK, et al. Trazodone and alcohol relapse: a retrospective study following residential treatment. Am J Addict . 2011;20(6):525-9.
36.Kishi T, Sevy S, Chekuri R, Correll CU. Antipsychotics for primary alcohol dependence: a systematic review and meta-analysis of placebo- controlled trials. J Clin Psychiatry. 2013;74(7):e642-54.
37.Bender S, Scherbaum N, Soyka M, Ruther E, Mann K, Gastpar M. The efficacy of the dopamine D2/D3 antagonist tiapride in maintaining abstinence: a randomized, double-blind, placebo-controlled trial in 299 a l c o h o l – d e p e n d e n t p a t i e n t s . I n t J N e u r o p s y c h o p h a r m a c o l .
2007;10(5):653-60.
***




