MAKING CONTRACTS – A VALUABLE METHOD IN ALCOHOL DEPENDENCE PSYCHOTHERAPY
Abstract
This article presents a very important part of alcohol abuse therapy, which is to establish the contact and the therapeutical objective. We propose, following our practice, the Transactional Analysis frame of reference. According to it, most part of the success or failure of psychotherapeutic process depends on contracting. Here we will present how using contracting, as a fundamental method of Transactional Analysis that can be used in alcohol abuse therapy. We prove that contracting must be the first step in every therapy, because it provides focus and clarity in management of the therapeutic process.
INTRODUCTION
Anterior skull base meningiomas represent between 12 and 22% of intracranial meningiomas and may originate in dura of orbital roof, olfactory groove and suprasellar structures (tuberculum sellae, planum /jugum sphenoidale, anterior clinoidian process), the most common being the olfactory groove tumors, followed by the tuberculum sellae ones (1). Olfactory meningiomas may progress silently for a long time; headache is the most common symptom at presentation; although anosmia occurs in 85-90% of cases is rarely the presenting symptom; as the tumors grow, become apparent the clinical manifestations of pressure on the frontal lobe including mental symptoms that often lead to misdiagnosis and psychiatric therapy. Suprasellar meningiomas develop in the vicinity of optical structures, causing early and progressive alterations of vision in 90-
99% of cases thus the diagnosis of is earlier than in olfactory groove meningiomas; other relatively common symptoms in these tumors are headache, epilepsy and psychiatric disorders. As a consequence, depending on the location, the anterior skull base meningiomas may manifest by or associate psychiatric disorders caused by compression over the frontal lobe (2).
MATERIALAND METHODS
Our retrospective study was conducted on 64 meningiomas of the anterior floor of the skull base diagnosed between 2007-2013 at the National Institute of Neurology and Neurovascular Diseases, Neurosurgery clinic, that were evaluated in terms of clinical manifestations, particularly psychological symptoms. Imaging diagnosis of these tumors was obtained by computed tomography and magnetic resonance imaging w i t h a n d w i t h o u t c o n t r a s t a n d c o n f i r m e d b y histopathological examination of surgically removed specimens. The operative technique consisted of unilateral and bilateral frontal approach and pterional approach for selected cases. Clinical data of interest were obtained from registers of investigations and patient’s observation sheets.
RESULTS
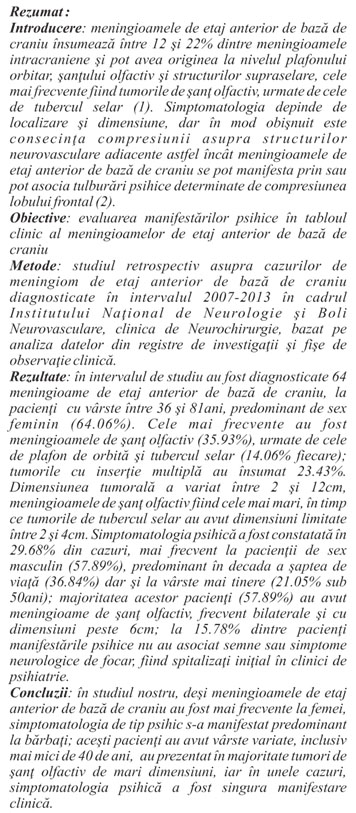
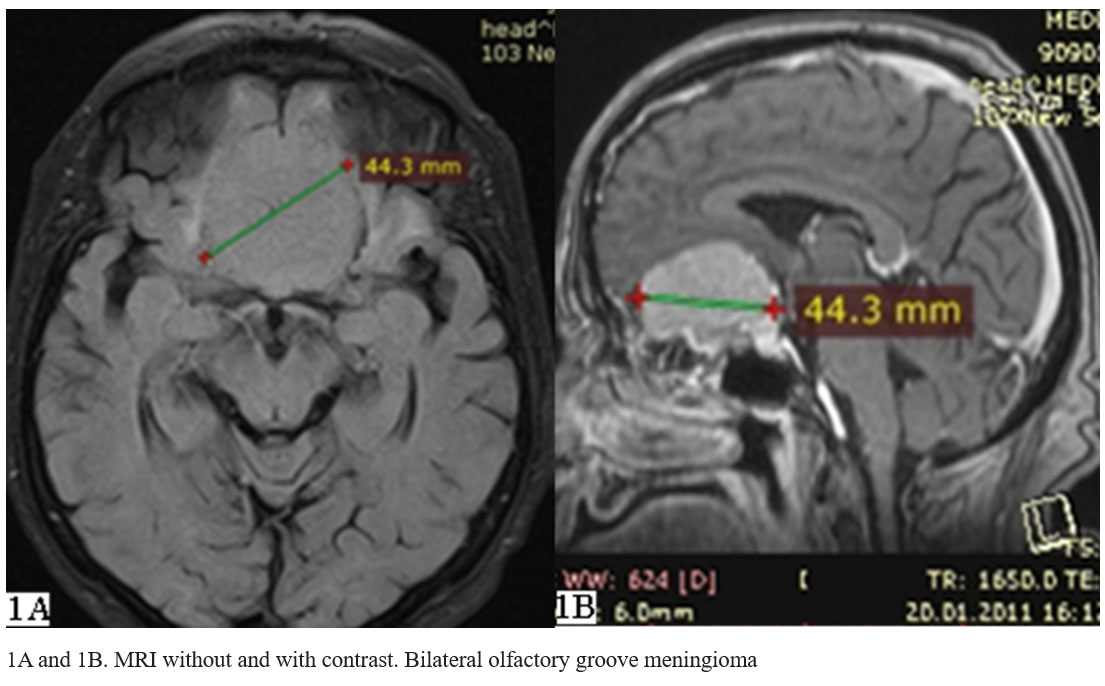
The 64 anterior skull base meningiomas diagnosed in 2007-2013 period were from 41 women (64.06%) and 23 men, female/male ratio of 1.78/1, aged between 36 and 81years (Table 1).
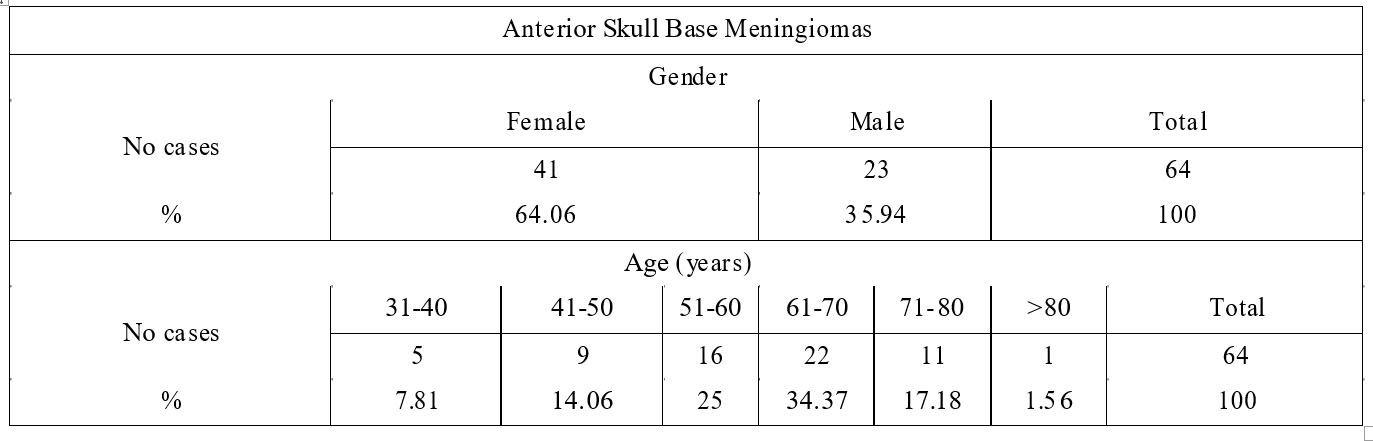
Table 1. Distribution of meningiomas by gender and age
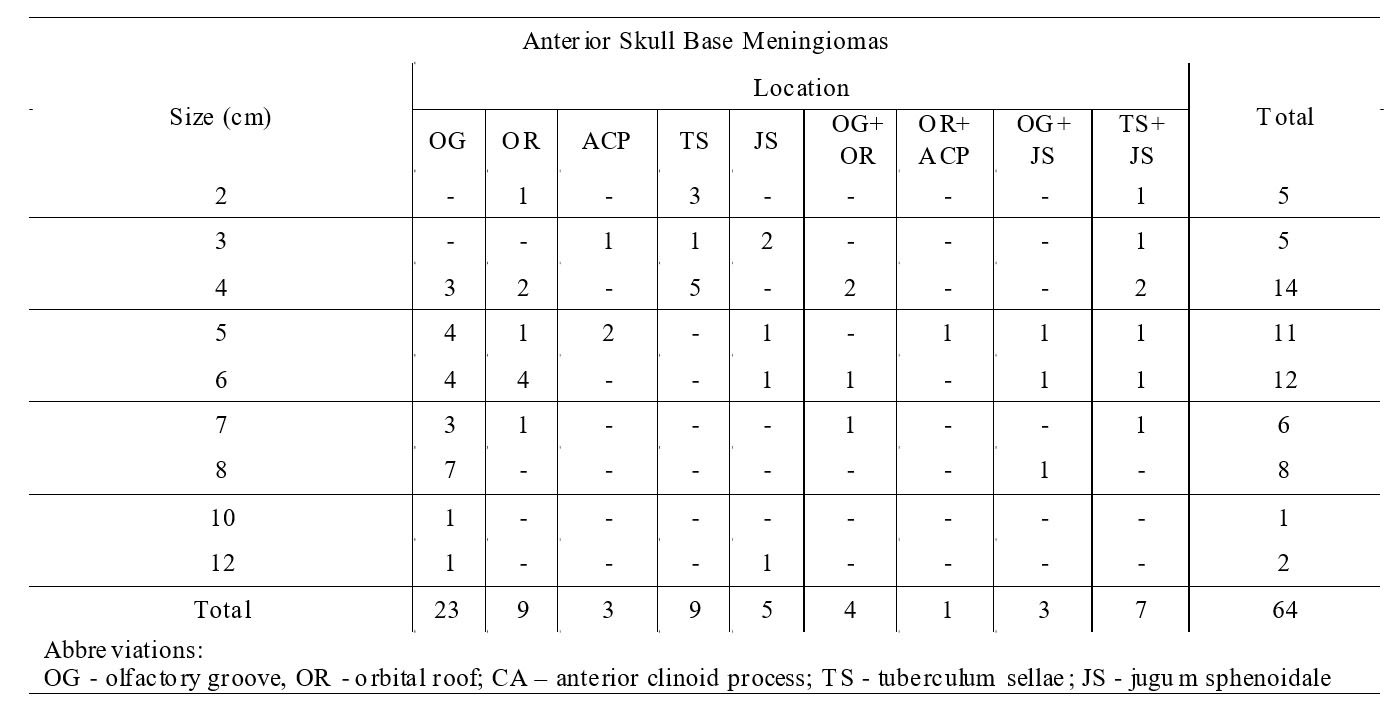
Table 2. Distribution of meningiomas by size and location
Most of the 64 meningiomas, summing 22 cases
(34%) were diagnosed in patients in the range of age of 61
70 years, followed as frequency by patients between 51 and 60 years (25%). These tumors were also found in younger patients less than 40 years (5 cases, 7.8%).
Imaging diagnosis of these tumors has been obtained by computed tomography and /or magnetic resonance imaging, with and without contrast, which has been used to determine the insertion /location and size of tumor, the imaging features indicative for meningiomas and the effects of tumors on adjacent neurovascular structures.
The radiographic appearance of meningiomas consisted in well-defined masses with smooth contour and strong homogenous enhancement with contrast, located on the anterior skull base, with insertion and growth on one or both side of the median plane. Characteristic of meningiomas was tapered extension of the enhanced mass into the surrounding dural base (“dural – tail); there were also revealed certain morphological features of the tumor (as vascularity, calcifications, cysts) and the presence of peritumoral edema or hyperostosis. Magnetic resonance imaging provided significant details about the relation of tumor with the adjacent neurovascular structures (frontal lobe, cerebral arteries, optic nerve, optic chiasm, pituitary stalk), important in determining of therapeutic plan.
The goals of surgery abord were the complete excision of the tumor with involved dural attachment and preservation of the surrounding neurovascular structures; it consisted in unilateral frontal approach in 53 cases, bilateral frontal approach in 7 cases and pterional approach in those 4 cases of anterior clinoidian process meningiomas.
Topographic, the 64 anterior skull base meningiomas were grouped in tumors of olfactory groove, orbital roof, anterior clinoid process, tuberculum sellae and planum/ jugum sphenoidale; we also noted cases with multiple insertion. The size of these tumors ranged between 2cm and 12cm (Table 2).
The most common were olfactory groove meningiomas found in 23 cases (35.93%); they were bilateral in a significant number (11 of 23). These tumors were generally large, ranging from 4 to 12cm (1 case), most with a diameter of 8cm (7 cases, 34.78%) (Figures 1A and 1B).
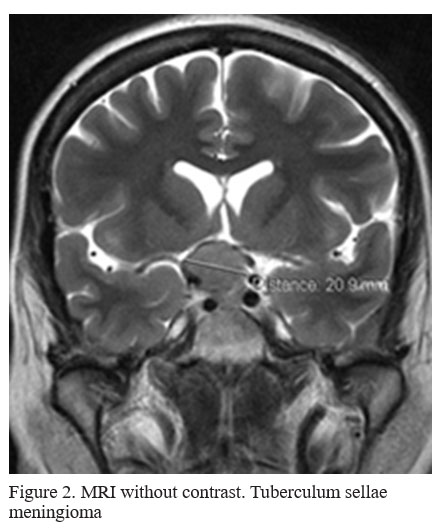
As frequency, followed the orbital roof and tuberculum sellae with 9 cases each (14.06%). The orbit roof meningiomas were generally large, 7 of them (77.77%) having the diameter of 4 to 6cm, while all 9 tuberculum sellae tumors were small sized, between 2 and 4cm (Figure 2).
More rare were jugum sphenoidale tumors found in 5 cases (7.81%) and ranging between 3cm (1 case) and
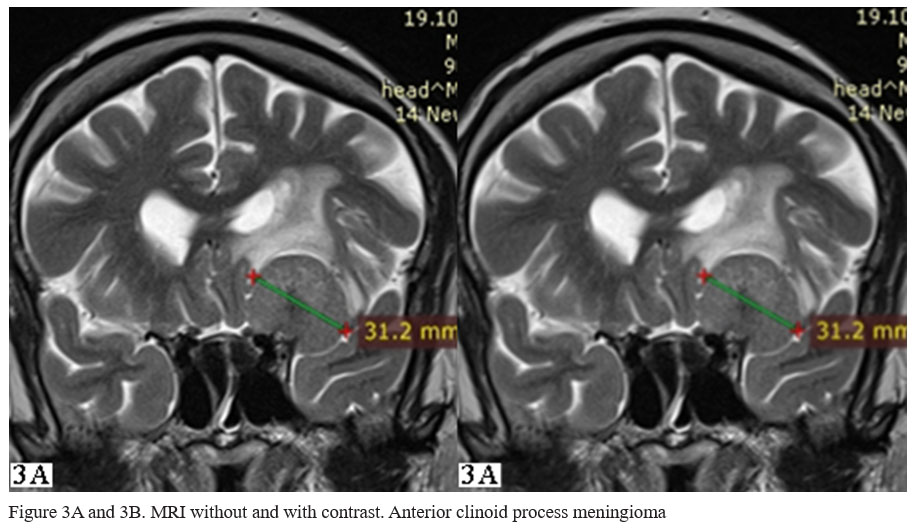
12cm (1 case) and anterior clinoid process meningiomas summing 3 cases (4.68%) and having diameters up to 5cm (Figure 3A and 3B).
Meningiomas with multiple insertions were relatively common, summing 15 cases (23.43%) and involving any two of the mentioned locations.
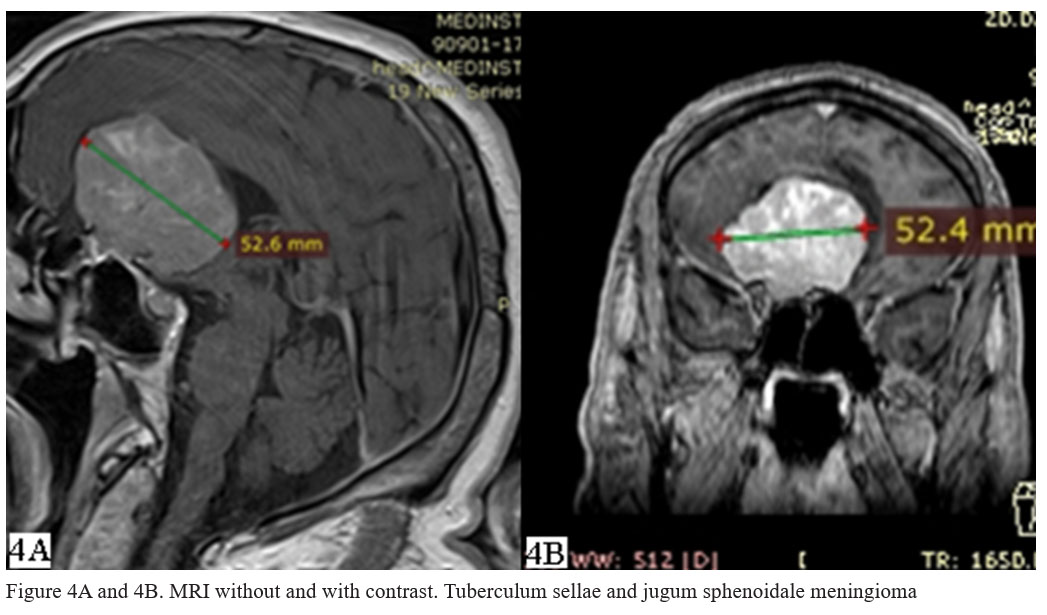
Among these, most frequent were tumors originated in tuberculum sellae and jugum sphenoidale, found in 7 of the 15 cases and having between 2 and 7cm in size (Table 2, Figure 4A and 4B).
Among the tumors with multiple insertions we also found olfactory groove and orbital roof meningiomas (2nd as frequency, with 4 cases), olfactory groove and jugum sphenoidale meningioma (3 cases) and orbital roof and anterior clinoid process meningioma (one case) (see Table 2).
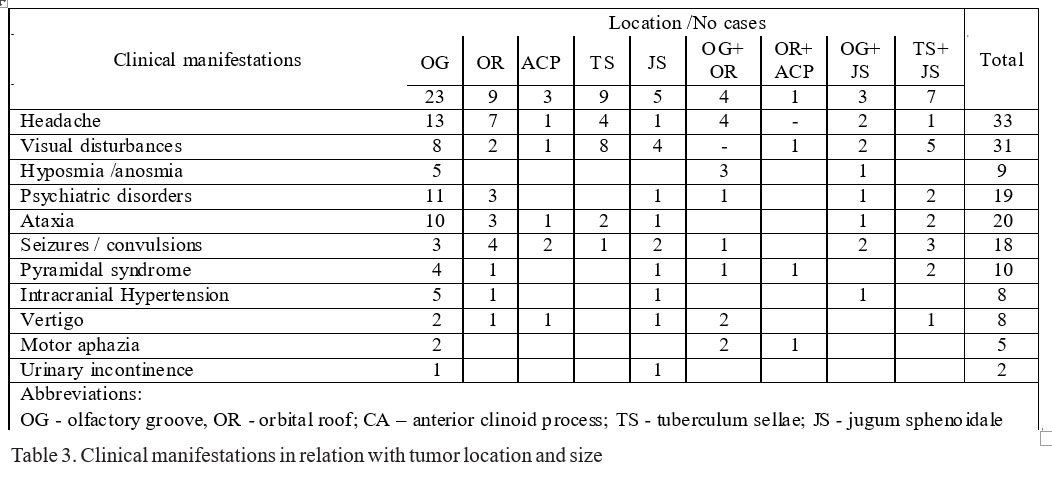
Clinical, the symptomatology associated with meningiomas was variable (Table 3):
Headache and visual disturbances dominated the clinical presentation regardless of tumor location, being reported in 33 (51.56%) and 31 cases (48.43%) respectively. Most patients with tumors of the orbit roof had headache (7 of 9 cases, 77.7%), while the visual disturbances predominated in tuberculum sellae tumors (8 out of 9 cases, 88.8%) as well in tumors with multiple insertion including tuberculum sellae, respectively in 7 of the 10 such cases (70%).
20 of the 64 patients (31.25%) presented with gait and balance disorder (ataxia), mostly (10/20 cases) having olfactory groove meningiomas; they represented also 43.47% of patients with tumors in this location (see Table 3).
Also common were manifestations described as loss of consciousness /seizures that summed 18 cases (28.12%), generally found in patients with large tumors for location; these were frequent in patients with tumors of orbital roof (4 of 5 cases, 80%), anterior clinoid process (2 of 3 cases, 66.6%) and jugum sphenoidale, including tumors with multiple insertion (9 of 15 cases, 60%).
More rare were manifestations such as pyramidal syndrome (10cazuri, 15.62%), intracranial hypertension (8 cases, 12.5%) that prevailed in patients with large tumors for location and vertigo (8 cases, 12.5%).
Smell disorders were rare and completed exclusively the clinical presentation of olfactory groove meningiomas in all the 9 cases (14.06%). Motor aphasia has been found occasionally (5 cases, 7.81%) especially in olfactory groove tumors, as was urinary incontinence (2 cases, 3.12%) affecting patients with frontal lobe mental disorders (Table 3).
Changes in behavior and personality, alterations of affectivity, memory and attention, reported as frontal lobe mental disorders were found in 19 cases (29.68%) (Table 3).
That psychiatric symptomatology predominated in males (11cazuri, 57.89%) and affected patients aged between 36 and 77 years, mostly in 7th decade of life (7 cases, 36.84%); 4 (21.05%) of the patients with frontal lobe mental disorders were under 50 years (Table 4).
In the absence of other neurological symptoms, 3 patients with psychiatric disorders (15.78%) were initially hospitalized in psychiatric clinics, but the symptoms persisted under specific therapy.
The symptoms has been described as installed gradually over several months or years (range, 3 months – 2 years), tumors reaching large size up to 6cm and more in most of the cases (15 of 19 cases, 78.94%) (see Table 4).
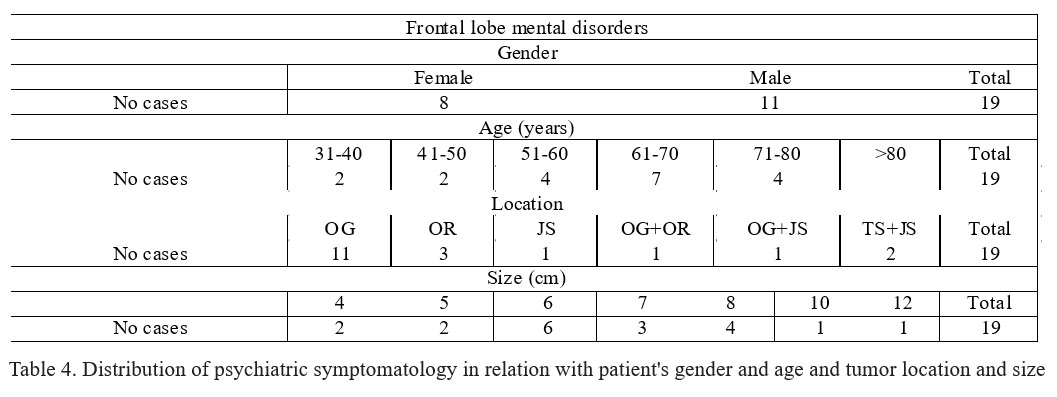
Referring to location, the vast majority of patients with frontal lobe mental disorders had olfactory groove meningioma, summing 11 of the 19 cases (57.89%) and also 11 of 23 patients with tumors in this location (47.82%). Other 3 cases (15.78%) were in patients with orbital roof tumors in which frontal lobe mental disorders were found with a frequency of 33.33% (3 of 9 cases). Rarely, patients with psychiatric symptomatology had tumors at other sites, including sphenoidal jugum and with multiple insertions (see Table
3 and Table 4).
DISCUSSIONS
For the 64 anterior skull base meningiomas diagnosed in 2007-2013 period we evaluated retrospectively data referring to patients gender and age, tumor location and s i z e a n d c l i n i c a l m a n i f e s t a t i o n s , p a r t i c u l a r l y psychological symptomatology.
In our study the anterior skull base meningiomas were found more frequently in women (64.06%), with a female/male ratio of 1.78/1 and affected mostly the 61-70 years age group, with a incidence of 34%, results that are in accord with similar studies that reported a predominance of anterior skull base meningiomas in women (female /male ratio of 1.4-2.6/1) and a maximum of incidence in 6 and 7 decades of life (3, 4). In our study, these tumors also affected patients under 40 years (7.8%), the younger having 36 years old.
As location, predominated olfactory groove meningiomas (23 cases, 35.93%) that were frequently bilateral tumors (47.82%), followed by the orbital roof and tuberculum sellae tumors, with 9% each; more rare were tumors of jugum sphenoidale (5 cases, 7.81%) and anterior clinoid process (4.68%). These results are partial similar to those revealed in study of Rubin et al., in which the most common were olfactory groove meningiomas (46%) followed by tuberculum sellae tumors (37%); the orbital roof meningiomas were among the most rare (3%) (1). In our study, a significant proportion was represented by tumors with multiple insertion (15 cases, 23.43%), among which the most frequent were meningiomas of tuberculum sellae and jugum sphenoidalle (7 of 15 cases).
Tumor size was between 2cm and 12cm; most of olfactory groove meningiomas (34.78%) were of 8cm in diameter; maximum size of 12cm was found in two cases, one of olfactory groove and one of jugum sphenoidale;
77.77% of orbital roof tumors were between 4 and 6cm; tuberculum sellae meningiomas were generally small tumors with size of 2-4cm.
Because of subfrontal location and slow rate of growth, olfactory groove meningiomas can reach very large sizes exceeding 6cm in most of cases, before the onset of clinical manifestations (5, 6). Bernhard et al. reported that through pressure on frontobasal lobe, the anterior skull base meningiomas may manifest with urinary incontinence and psychological symptoms including personality disorders, psychomotor disabilities and cognitive disorders (2).
We f o u n d p s y c h i a t r i c s y m p t o m a t o l o g y described as frontal lobe mental disorders in 29.68% of cases, with insidious onset over several months / years (3 months – 2 years) and predominating in males (57.89%, ratio 1.57/1). These patients were in 36-77years range of age, mostly between 61 and 70 years (36.84%), but with a significant proportion (21.05%) aged less than 50s. 15.78% of patients with clinical picture dominated by physical manifestations were initially treated in psychiatry.
In a similar study, Gupta and Kumar, reported psychiatric symptomatology in 21% of patients with meningiomas; these symptoms were present in 35% of men with meningiomas but in only 15% of women; average age at diagnosis was 60.5 years (7).
In our study, the majority of anterior skull base meningiomas manifested with psychological symptoms of frontal lobe were olfactory groove tumors (57.89%), often bilateral and large sized between 6 and 12cm; this symptomatology affected 47.82% of patients with tumors in this location.
Similarly, in series of Hentschel and DeMonte (8) and Bassiouni et al (9), mental disorders and disinhibited behavior, personality disorders and memory impairment were reported as early symptoms in 20-70% of patients with olfactory groove meningiomas, commonly attributed to aging or neglected by younger patients, but often noted by the family members.
15.78% of the remaining patients with psychiatric manifestations had orbital roof tumors; these symptoms affected 33.33% of the patients with tumors in this location. On the other hand, we found that suprasellar meningiomas, including tumors with multiple insertions, have manifested by psychiatric symptomatology more rarely than olfactory tumors (21.05% vs.57.89%).
Mumoli et al. stated that meningiomas with compressive effect on the frontal lobe are clinically silent for a long period, with a high probability of being overlooked or misdiagnosed because of the associated psychiatric symptoms that resemble to depression, anxiety, hypomania and schizophrenia (10). In contrast, in suprasellar tumors that arise in the vicinity of optical structures, visual symptoms are common and occur early leading to their precocious diagnosis; in these tumors, mental disorders are rare (11, 12).
In our study, cases presented with frequent mental symptoms, represented in the vast majority by olfactory groove and orbital roof tumors, the associated clinical manifestations were variable. In olfactory groove tumors, we often found symptoms as headache (56.52%) and ataxia (43.47%); anosmia was much less common (14.06%) and urinary incontinence was incidental (3.12%). In orbital roof meningiomas, associated clinical manifestations included headache (77.77%), loss of consciousness /seizures (44.44%) and ataxia (33.33%). In both of these types of tumor the psychiatric symptomatology predominated over the visual disturbances (47.82% vs. 34.78% and 33.33% vs. 22.22% respectively).
In the study of Fox et al. on the olfactory groove meningiomas, most patients developed one or a combination of the following clinical manifestations: subtle mental disorders, cognitive and personality changes, headache, visual disturbances and or seizures (13), while visual symptoms and dementia were the main events at presentation in the series of Bakay and Cares (14); Ojemann reported mainly subtle mentally deficit and headache, while visual disturbances were relatively rare (15).
CONCLUSIONS
Psychiatric symptomatology may be the main manifestation in anterior skull base meningiomas so that t h e s e t u m o r s m a y i n i t i a l l y b e o v e r l o o k e d o r misdiagnosed. In our study, although these tumors were more common in women, psychiatric symptoms were found predominantly in males; the affected patients were of various ages including under 40s and had large and often bilateral olfactory groove tumors in the great majority of cases; a significant proportion of these patients were initially diagnosed with psychiatric pathology.
Abbreviations: OG – olfactory groove, OR – orbital roof; CA – anterior clinoid process; TS – tuberculum sellae; JS – jugum sphenoidale
REFERENCES
1.Rubin GU, Ben D, Gornish M, Rappaport ZH. Meningiomas of the anterior cranial fossa floor. Review of 67 cases. Acta Neurochir 1994;129: 26-30.
2.Bernhard R, Brokinkel F, Brokinkel B. Surgical Management of Skull Base Meningiomas – An Overview. In: Monleon D (ed.). Meningiomas – Management and Surgery. InTech Editure, 2012, 5-102.
3.Park BJ, Kim HK, Sade B. Epidemiology. In: Lee JH (eds). Meningiomas. Diagnosis, Treatment, and Outcome. London: Springer- Verlag, 2008, 11-15.
4.CBTRUS. Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2004-2008. (March 23,
2 0 1 2 R e v i s i o n ) h t t p : / / w w w . c b t r u s . o r g / 2 0 1 2 – N P C R – SEER/CBTRUS_Report_2004-2008_3-23-2012.pdf
5.Turazzi S, Cristofori L, Gambin R et al. The pterional approach for the microsurgical removal of olfactory groove meningiomas. Neurosurgery 1999;45: 821-826.
6.Hentschel SJ, Demonte F. Olfactory Groove Meningiomas. Neurosurg Focus 2003;14(6): 128-133.
7.Gupta RK, Kumar R. Benign brain tumours and psychiatric morbidity: a 5-years retrospective data analysis. Aust N Z J Psychiatry 2004;38: 316.
8.Hentschel SJ, DeMonte F. Olfactory groove meningiomas. Neurosurg Focus 2003;14(6): 144-149.
9.Bassiouni H, Asgari S, Stolke D. Olfactory groove meningiomas: functional outcome in a series treated microsurgically. Acta Neurochir 2007;149: 109–121.
10.Nicola M, Pulerà F, Vitale J, Camaiti A. Frontal lobe syndrome caused by a giant meningioma presenting as depression and bipolar disorder. Singapore Med J 2013;e54(8): e158-e159.
11.Tuna H, Bozkurt M, Ayten M, Erdogan A, Deda H. Olfactory groove meningiomas. J Clin Neurosci 2005;12: 664–668.
12.Gokalp HZ, Arasil E, Kanpolat Y et al. Meningiomas of the tuberculum sella. Neurosurg Rev 1993;16(2): 111–4.
13.Fox D, Khurana VG, Spetzler RF. Olfactory Groove/Planum Sphenoidale Meningiomas. In: Lee JH (eds). Meningiomas. Diagnosis, Treatment, and Outcome. London: Springer-Verlag Limited, 2008, 327- 332.
14.Bakay L, Cares HL. Olfactory meningiomas. Report on a series of twenty-five cases. Acta Neurochir 1972;26: 1–12.
15.Ojemann RG. Olfactory grove meningiomas. In: Al Mefty O (ed). Meningiomas. New York: Raven Press, 1991, 383–94.
***



