THE SOMATIC COMORBITIES TO DEPRESSED ELDERLY
Abstract
Introduction: Elderly people with depression often associated medical comorbidities. The association between depression and somatic diseases lead in dificulties of diagnosis because depressive symptoms are frequently attributed to comorbidities. Objective: The study aims to identify the main comorbidities co-existing with depression in the elderly population and to follow-up the temporal ratio between somatic and depression onset and vice versa. Material and method: This was a restrospective study that included elderly patients with depression. The study was conducted for 2 years and the patient selection was made at the time of presentation to a psychiatrist for an episode of major depression. The inclusion criteria were: age> 65 years, diagnosis of major depression and the presence of medical comorbidities. Results: It were identified a total of 513 elderly patients with major depression. Of these, a total of 466 patients (91.02%) already had a diagnosis of major depression at the time of assessment and a number of 46 patients (8.98%) were not diagnosed with depression before inclusion in the study. When depression was installed prior to onset of somatic desease depression was noticed mostly on females (n = 36; 78.26%) than males (n = 10; 21.73%), p <0.0001. In patients in which depression occured after the onset of somatic disease, the age of onset of depression was 69.48 ± 7.09. Most depressive episodes have been experienced by the patients with 6 associated comorbidities, (2.40 ± 0.89) but the differences were not significant between groups. Conclusions: Depression in the elderly is associated with an increased incidence of medical comorbidities, is more prevalent in women, and the length of time elapsed between the onset of somatic disease and the occurrence of depression is dependent on the number of depressive episodes, number of associated comorbidities and the presence of cardiovascular disease.
INTRODUCTION
The origin of depression in the elderly is based on multiple causes including psychological factors, social and biological complementarity may induce depressive symptoms in this population.
Unlike younger persons with depression, elderly persons with depression usually have a medical comorbidity (1, 2). Major depression is more common in medically ill patients who are older than 70 years and hospitalized or institutionalized (3). Severe or chronic diseases associated with high rates of depression include stroke (30 to 60 percent), coronary heart disease (8 to 44 percent), cancer (1 to 40 percent), Parkinson’s disease (40 percent), Alzheimer’s disease (20 to 40 percent), and dementia (17 to 31 percent) (3).
From the clinical point of view, the association between depression and somatic diseases lead in dificulties of diagnosis because depressive symptoms are frequently attributed to comorbidities (4-7). More than treating depression in this category of patients is difficult due to the side effects that some antidepressants may o c c u r , a g g r a v a t i n g s o m a t i c e v o l u t i o n . . In examining the connection between depression occurring in the elderly and medical comorbidities that are often associated with, two distinct situations should be analised.
First , depression is installed later than medical comorbidities and this reflects both general mechanisms related to stress and disability as well as more specific physiological mechanisms related to cerebrovascular disease clinical unfold yet , endocrine and metabolic effects (8-10). Similarly, the somatic disease which appear subsequently depression include general mechanisms related to self -neglect , poor adherence to medical treatments and maladaptive behaviors to health or specific physiological mechanisms related to the endocrine or autonom nervous system malfunction .The two situations coexist in clinical practice is a vicious circle.
The coexistence of medical illness and depression is less common in younger people but increases substantially with age (11-15).
Data from the literature provides information on the high prevalence of depression in older people with medical comorbidities. The previous studies are focused on clarifying the mechanisms underlying this inter- relationships but do not provide data about the impact of depression on the development of somatic diseases , about particularities of gender or if the number of associated comorbidities may influence the emergence of depression in the elderly (13-16).
OBJECTIVE OF THE STUDY
T h e s t u d y a i m s t o i d e n t i f y t h e m a i n comorbidities existing with depression in the elderly population in a given population group (Câmpulung Mușcel – Arges) and follow the temporal ratio between somatic and depression onset and vice versa.
Secondary endpoints of the study were the analyse of the relationship between the number of comorbidities associated, the average time between the onset of comorbidities to the onset of depression and severity of depression.
MATERIALAND METHOD
This was a restrospective study that included elderly patients with depression who were registered in the Câmpăulung Muscel psychiatry database . The study was conducted between 01.jan.2010-31.dec.2011 and the patient selection was made at the time of presentation to a psychiatrist for an episode of major depression.
The inclusion criteria were: age> 65 years, diagnosis of major depression and the presence of medical comorbidities. For the accuracy of the results were included in the study only patients in which depression was diagnosed after the age of 55 years. Questionnaires used to diagnose depression were DSM IV and ICD 10 and the intensity of depression was evaluated with MADRS, HAM-D and CGI.
After obtaining verbal and written informed consent of the patient and a a caregiver of him it were recorded patient data as age at enrollment, gender, origin, age of onset of somatic diseases and type, age of onset of depression, number of depressive episodes, the gap between the onset of somatic illness and depression or between onset of depression and the emergence of somatic disease.
Statistical analysis of data was performed using STATISTICA 8.0.
Student test was used to compare numerical variables between the two groups, ANOVA test for comparison of numerical variables between multiple groups, chi-square test to compare qualitative variables. Univariate and multiple regression analysis was performed to establish the main predictors for time elapsed between the onset of somatic disease and diagnosis of depression in elderly.
Statistical significance was set to ap value <0.05.
RESULTS
During the entire period of the study it were identified a total of 256 elderly patients with major depression. Of these, a total of 466 patients (91.02%) already had a diagnosis of major depression at the time of assessment and a number of 46 patients (8.92%) were not diagnosed with depression before inclusion in the study. The characteristics of elderly patients with depression are showed in table nr.1
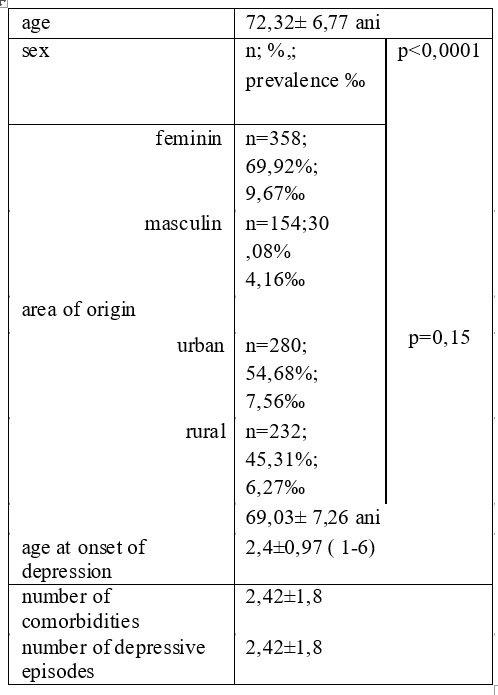
Table 1. Characteristics of elderly patients with depression
Analysis of the relationship between depression and somatic disease onset showed a very low number of 46 (8.98%) of patients in which depression was installed prior to onset of somatic disease and a number of 466 patients (91.02%) in which depression was installed after the appearance of somatic disease (p <0.0001).
THE ONSET OF DEPRESSION PRIOR SOMATIC DISEASES
Depression was noticed that mostly on females (n = 36, 78.26%) than males (n = 10, 21.73%), p <0.0001, and were significant difference in the area of origin (n=18;39,14% rural versus urban n= 28, 60.86%, p = 0.40). The average time elapsed from the onset of depression to somatic disease was 5.47 ± 5.63 years and the number of associated comorbidities was 2.30 ± 0.70.
The main medical comorbidities recorded in these patients are shown in Table 2.
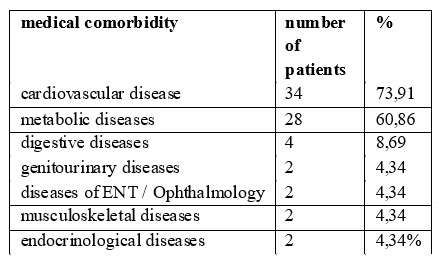
Table 2. Medical comorbidities in patients with depression
ENT= ears-nose and throat
THE ONSET OF DEPRESSION AFTER SOMATIC DISEASE
Mean age at baseline was 72.09 ± 6.69 years. Gender distribution of patients in which the onset of depression was after somatic disease showed a predominance of females (n = 161, 69.1%) than males (n = 72, 30.9%), p <0.0001.
There were no significant differences in the area of origin (45.9% versus 54.1% rural from urban, p = .23).
Age of onset of depression was 69.48 ± 7.09 and the length of time between onset of illness and depression was 5.19 ± 3.46 years. Number of depressive episodes recorded before the onset of depression at baseline was on average 2.19 ± 1.14.
Regarding associated comorbidities it were recorded between 1-6 somatic diseases associated , average 2.41 ± 0.99. The main comorbidities recorded are shown in Table 3.
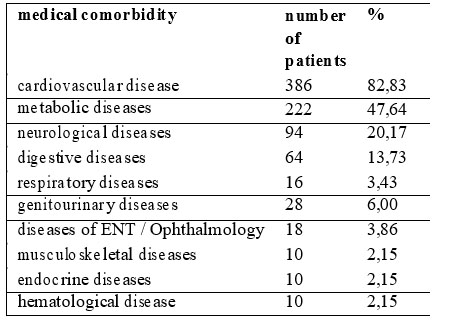
Table 3. Medical comorbidities in patients with depression diagnosed after somatic diseases
The most common association found in patients with depression are shown in Table no.4
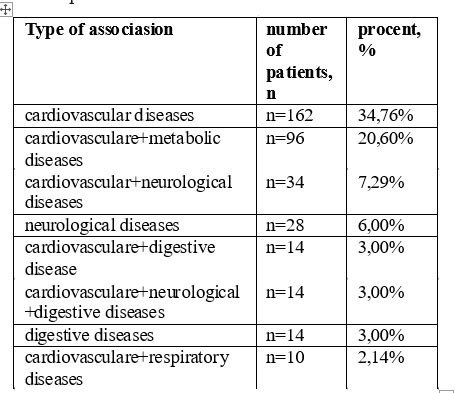
Table 4. Association between somatic diseases more frequently encountered in the analyzed group
The difference of time between the disease onset and depression diagnosis, depending on the type of disease is shown in table no.5
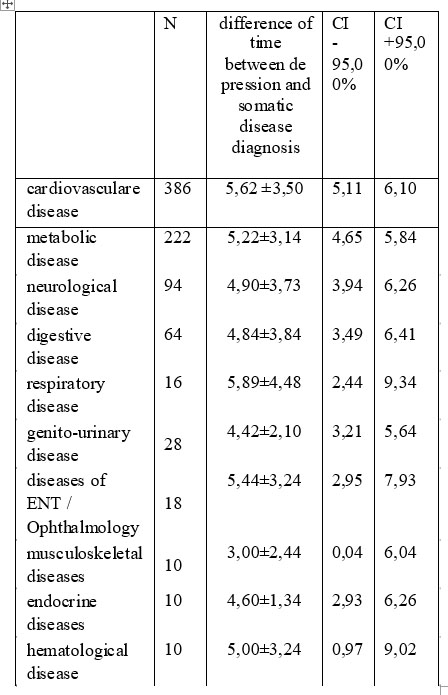
Table 5. The difference of time between the disease onset and depression diagnosis
N=number of patients, CI=confidence interval.
Hypertension was the most frequently detected (79.39%, n = 370), followed by coronary artery disease (41.63%, n = 194) and dyslipidemia (34.33%, n = 160). A history of diabetes was recorded at a number of 74 patients (15.87%).
M o s t d e p r e s s i v e e p i s o d e s h a v e b e e n experienced by the patients with 6 associated comorbidities, (2.40 ± 0.89) but the differences were not significant between groups (figure no.1).
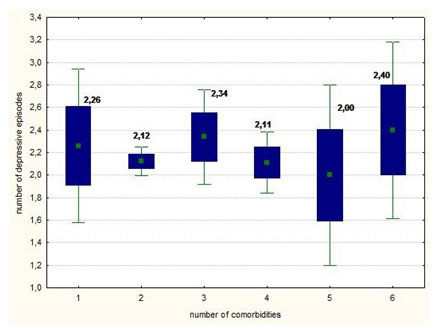
Fig. 1. Number of depressive episodes according to the number of co-morbidities associated
Also, there were no significant differences in the length of time until the onset of depression between the two sexes by the number of comorbidities associated, as shown in figure no.2.
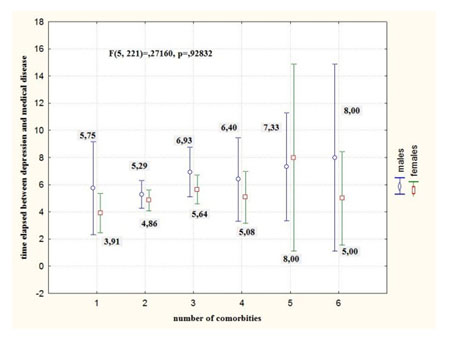
Fig. 2. The elapsed time between the onset of depression and the number of comorbidities associated by sex
It were no significant differences between the number of depressive episodes the type of comorbidity However, univariate analysis demonstrated a significantly more variability in the number of depressive episodes in patients with a history of neurological disease (SS = 8.21, F = 6.34, p = 0.01).
Multiple regression analysis with the time difference to the appearance of depression as the dependent variable and the number of associated co- morbidities, no. of depressive episodes and type of somatic disease showed that the number of depressive episodes, number of associated comorbidities and cardiovascular disease are independent predictors of the time elapsed from the occurrence of somatic disease to onset depression (p <0.004). (Table 6).
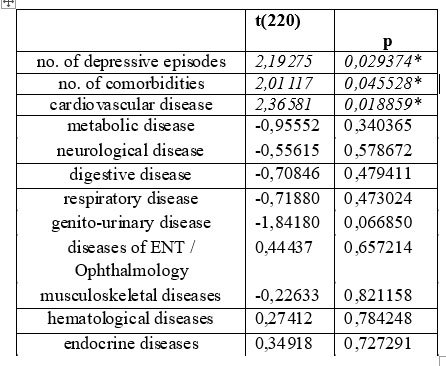
Table 6. predictors of time elapsed between somatic disease and depression
DISCUSSIONS
Many of elderly patients (10-25%) with chronic disease are suffering of major depression. In fact, there is a direct relationship between depression and medical comorbidity, knowing that patients with depression have an increased association with chronic diseases (1-10).
Our results showed that in most cases, depression was installed after the occurrence of somatic disease. Such were identified only 46 patients whose somatic disease began after the onset of depression. The results should be interpreted with caution and only in respect of the statistical significance on the same background. Depression has an negative influence on the development of somatic diseases and difficult recovery and the somatic disease is a trigger for depression.
Thus, patients with depression who have somatic diseases have a higher death rate and a lower life expectancy, which may explain their less numerous representation in the studied group.This observation is supported by the fact that in the analyzed group, the time from the appearance of somatic depression was short in most cases (1-2 years) and depression was classified as mild in 78.26% of cases (n = 36).
After analyzing the results, we observed high prevalence of depression in elderly female patients compared to males (p <0.0001).
Major depression is more common in females and this observation is maintained in elderly..One of the explanations is a higher survival rate of women compared to men (17-18).
Future studies conducted on age-matched subjects but different sex should be performed to afirm the higher incidence of depression in elderly women than men .
In a study conducted by Takkinin et al. in 2004 it was reported a higher incidence of depressive symptoms in women compared to men (19).
T h e d i ff e r e n c e s a r e h i g h e r w i t h a g e . In our study there were no statistically significant differences between patients from rural and urban areas in terms of the number of elderly patients with depression (45.9 % versus 54.1% rural from urban , p = 0.23 . It was observed an increased incidence of cardiovascular disease ( 82.83 %) , metabolic ( 47.64 %) and neurological diseases ( 20.17 %). Hypertension was detected most frequently ( 79.39 %, n = 390 ) , followed by ischemic heart disease ( 41.63 %, n = 194 ) and dyslipidemia ( 34.33 %, n = 160). Medical history of diabetes were recorded for a total of 37 patients ( 15.87 %). The presence of increased incidence of medical pathology in elderly people with major depression converge to the theory of vascular depression in the elderly.
Our results may differ from results of a study published in 2003 that quantified the medical comorbidities associated with depression in elderly patients hospitalized for major depression. The depressed elderly patients had high medical comorbidity,and most required follow up medical care. The results of the study showed that about 75% of patients had at least one comorbid condition requiring treatment; 46% had two or more,and 25% had three or more conditions requiring treatment. The mean number of comorbid medical conditions scored at two or higher (reflecting need for treatment) was 1.6 .This study found an incidence of cardiovascular disease by 63.1% , 46.21 % of the metabolic and 40.5 % of the neurological and indicate a higher incidence of musculoskeletal diseases 48.2% (20).
There could not be established a significant correlations between the number of co-existing comorbidities with the distance of time between the onset of somatic illness and depression and the number of depressive episodes. Instead somatic type and combination type significantly influenced the mentioned parameters.
Thus, the multiple regression analysis for the time elapsed to onset of depression as the dependent variable and the number of associated co-morbidities , no. depressive episodes and type of somatic disease showed that the number of depressive episodes , number of associated comorbidities and cardiovascular disease are independent predictors of the time elapsed since the occurrence of somatic disease to the onset depression ( p < 0.004).
CONCLUSIONS
Depression in the elderly was associated with an increased incidence of medical comorbidities, the most common being cardiovascular disease, in particular hypertension, metabolic diseases – dyslipidemia, diabetes and neurological diseases.
High incidence of hypertension, dyslipidemia and diabetes in elderly people with depression suggests the likelihood contribution of vascular lesions to the onset of depression.
Cases in which depression precedes somatic diseases in the analysed group are less numerous than those in which depression occurs at a variable time after the onset of somatic illness. This can be justified by the high mortality of this category of patients, leading to a reduced representation in the category of elderly patients.
Late-onset depression is more prevalent in women, and the length of time elapsed between the onset of somatic disease and the occurrence of depression is dependent on the number of depressive episodes, number of associated comorbidities and the presence of cardiovascular disease.
REFERENCES
1.Ganzini L, Smith DM, Fenn DS, Lee MA. Depression and mortality in medically ill older adults. J Am Geriatr Soc 1997;45: 307–12.
2.Callahan CM, Dittus RS, Tierney WM. Primary care physicians’ medical decision making for late-life depression. J Gen Intern Med 1996;11: 218–25.
3.Boswell EB, Stoudemire A. Major depression in the primary care setting. Am J Med 1996;101: 3S–9S.
4.Koenig H. Differences in psychosocial and health correlates of major and minor depression in medically ill older adults. JAGS 1997;45: 1487–1495.
5.Koenig HG, Meador KG, Cohen HJ, Blazer DG. Depression in elderly men hospitalized with medical illness. Arch Internal Med 1988;148: 1929–1936.
6.Ghebaur L, Prepeliceanu D. Tulburarea depresivã secundarã în practica clinicã psihiatricã. Revista Românã de Psihiatrie 2007;9: 16-20.
7.Mordechai M. Probleme de management în tratamentul depresiei la pacienții vârstnici. Med Con 2011;4: 117-120.
8.Krishnan KR. Depression as a contributing factor in cerebrovascular disease. Am Heart J 140(suppl 4): 70–76.
9.Kaimal AB, Nair UV. Organic brain dysfunction in late-onset depression. British Journal of Psychiatry 2005;187-288.
10.Lyness JM, Bruce ML, Koenig HG, et al. Depression and medical illness in late life: report of a symposium. J Am Geriatr Soc 1996;44: 198–203
11.Verbrugge L. Sex differences in health, in The Encyclopedia of Aging. New York: Springer, 1995, 850-854.
12.Rubin EH. Psychiatry and old age, in Adult Psychiatry. St. Louis: MO, Mosby, 1997, 395–405.
13.Stewart AL, Greenfield S. Functional status and wellbeing of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA 2001;262(7): 907–913.
14.Roose SP, Glassman AH. Relationship between depression and other medical illnesses. JAMA 2001;286(14): 1687–1690.
15.Grecu MG, Gabos GI, Moica Th, Vesa A, Grecu GC. Depression and psychosomatic diseases, 18th European Congress of Psychiatry, Munich, February 27 – March 2, 2010.
16.Consoli SM. Depression and Organic Diseases Study. Depression and associated organic pathologies, a still under-estimated comorbidity. Results of the DIALOGUE study. Presse Med 2003;32(1):10-21.
17.Hollon SD, Jarrett RB, Nierenberg AA, Thase ME, Trivedi M,Rush AJ.Psychotherapy and medication în the treatment of adult and geriatric depression: which monotherapy or combined treatment? J Clin Psychiatry 2005;66(4): 455-68.
18.Thornett AM, Mynors-Wallis LM. Credibility of problem-solving therapy and medication for the treatment of depression among primary care patients. Med Sci Monit 2002;8(3):CR193-6.
19.Takkinin S, Gold C, Pedersen B, Malmberg B, Nilsson S, Rovine M. Gender differences in depression: a study of older unlike-sex twins. Aging and Mental Health 2004;8: 187–194.
20.Proctor EK, Morrow-Howell NL, Dore´P et al. Comorbid Medical Conditions Amon Depressed Elderly Patients Discharged Home After Acute Psychiatric Care. Am J Geriatr Psychiatry 2003;11(3): 329-338.
***



