QUALITY OF LIFE IN DEPRESSION
Abstract
OMS defineşte “calitatea vieţii” ca percepţia individului asupra poziţiei sale în viaţă în contextul sistemului cultural şi de valori în care trăieşte şi în relaţie cu scopurile, aşteptările, standardele şi preocupările sale (3). Deşi reprezintă un concept cu o accepţiune atât de vastă şi subiectivă, calitatea vieţii este influenţată în mod complex de sănătatea fizică, starea psihologică, nivelul de i n d e p e n d e n ţ ă , re l a ţ i o n a re a c u c a r a c t e r i s t i c i l e proeminente ale mediului în care persoana activează. Depresia nu reprezintă numai o tulburare obişnuită, adesea cronică şi recurentă ci, este în mod esenţial asociată cu deteriorarea activităţii lucrative şi a stării de bine din punct de vedere social şi psihologic (4). Impactul depresiei asupra calităţii vieţii este influenţat de severitatea simptomatologiei, dar şi de o multitudine de alţi factori cum ar fi: prezenţa simptomelor algice şi a afecţiunilor comorbide, trăsăturile de personalitate, resursele financiare, accesibilitatea suportului social, realizarea scopurilor personale şi nivelul succesului personal. Unele aspecte ale depresiei pot fi considerate intangibile. Acestea includ durerea, suferinţa familiei, a persoanelor de îngrijire şi a prietenilor şi stresul suportat de aceştia precum şi alte tipuri de relaţionare care, deşi nu pot fi măsurate în mod direct se manifestă prin perturbarea activităţilor zilnice, a relaţiilor familiale şi a vieţii sociale. în general nu sunt incluse în estimările privind costurile depresiei, şi estimările formale ale costurilor depresiei atât ale celor directe cât şi ale celor indirecte. Cu toate acestea marea majoritate a intervenţiilor pentru tratamentul tulburării depresive majore sunt considerate cost-eficiente. (16). Acest lucru ar trebui să constituie un argument în plus pentru depistarea precoce şi tratamentul corect al tulburărilor de tip depresiv.
DEFINITIONS AND CONCEPTS:
In 1948 (1) World Health Organization (WHO) defined health as „a state of physical, mental and socialwell-beingand not merely the absence of disease.” In this context it becomes increasingly clear that to address a larger problem, that of restoring health, treatment of any disease should target improvement beyond the specific signs and symptoms. Achieving such standards involves targeting the achievement of some results both in terms of physical and mental health.
The term „quality of life” has been used increasingly more often and became such a „popular” term that led to a wider understanding of „wellness” including aspects of happiness and satisfaction with life as a whole (2).
There are many definitions regarding the quality of life and, although the term „quality of life” makes sense for almost everyone and is approached by many academic disciplines, its meaning varying more or less for each person or group. (2)
Most definitions of quality of life explicitly state that when evaluating quality of life, perception of the different circumstances in their lives should be considered in patients (1). This includes perceptions of social behaviour, physical health, functioning in daily activities and work, economic status and the general feeling of wellbeing. (1)
WHO defines „quality of life” as the individual’s perception of his position in life in the context of the cultural and value system in which they live and in relation to their goals, expectations, standards and concerns. (3)
Although it represents a concept with a vast and subjective acceptance, the quality of life is complexly influenced by physical health, psychological state, level of independence, the relationship with the prominent features of the environment in which the person operates. QUALITY OF LIFE IN RELATION TO HEALTH
The concept of quality of life in relation to health has been developed since the 80s and refers to those aspects of quality of life have been proved to clearly affect health either physically or mentally.(2)At the individual level, perception on physical and mental health and the elements with which they are correlated, such as: level of functioning, social support, socio-economic status are included. There are some health issues that seem not to hall-mark on the quality of life at the time of evaluation such as a genetic predisposition without clinical expression at the time of assessment, that is unknown to the subject. (2)
At Community level „quality of life in relation to health” includes resources, conditions, policies and practices that influence the perception of health and function.
Self-assessment of health status has been shown to be a stronger predictor of mortality and morbidity than other more objective measurements of health. (2)
Interpretation of these data may help to identify the needs of health policies and legislation concerning health, can help in making decisions regarding the allocation of resources, develop strategic plans and can monitor the effects of the interventions in the community. MEASURING QUALITY OF LIFE
In order to evaluate the quality of life,a plurality of parametershas been used over time .
It is considered:
-socio-professional status
-capacity/incapacity of performing the duty tasks
– capacity/incapacity to perform daily activities
-economic status
-existence of a support system
-existing comorbidities
-interpersonal relations and social involvement
WHO together with 15 collaborating centres have developed two tools specifically for measuring quality of life: WHOQOL-100 and WHQOL-BREF.(3) These scales have the advantage of providing a subjective vision that people have on how the disease affects their lives some corroborating several areas of interest to assess quality of life (physical health, psychological c h a r a c t e r i s t i c s , l e v e l o f i n d e p e n d e n c e , s o c i a l relationships, environment , spirituality / religion / personal beliefs). In the short WHQOL-BREF version, these areas were merged resulting in four major areas: physical, psychological, social relationships and environment.
Many published studies that evaluated different aspects of quality of life use separate scales that assess the degree of disability (in different areas: work / activities, social functioning, family relationships) and productivity ( lost days, unproductive days) or social functioning.
When quality of life is used to estimate the cost effectiveness of some treatments or interventions or health policies,the terms of ” Years of Healthy Life (YHL)” and ” Diasbility-Adjusted Life Years” ( DALYs) are often used.
QUALITY OF LIFE IN DEPRESSION
Depression is not only a common disorder, often chronic and recurrent, but is essentially associated with the degradation ofthe lucrative activity and of social and psychological well-being state.(4) Major Depressive Disorder is the fourth leading cause of disability worldwide and is projected to end up being the second leading one in 2020. (5) There are studies (The Medical Outcomes Study) whose results show that individuals with depression show a physical, psychosocial and role functioning comparable or worse than those who have chronic medical conditions. In addition, the more a patient remains symptomatic for a long time, the smaller the chances of recovery(4)(6) and therefore he associated dysfunction will be higher.
The impact on quality of life is related to the severity of depression.(6) Hence, severe depression has profound consequences on the social and economic level, often involving high percentage of complex comorbidities and mortality (eg. Increased risk of cardiovascular disease and unfavorable outcome of cardiovascular diseasesand sucide ), reduced quality of life and significant personal and social costs caused by lower labor productivity, absenteeism and use of health services.(6)
It results that depression, like other chronic medical conditions who are following a pattern of remissions and relapses are associated with two types of burden in connection with illness. The first category is represented by what the affected person feels and may include discomfort, pain or suffering, difficulties in performing daily activities. The second category is represented by the economic burden that includes the costs of providing health and social services, loss of productivity, the burden given to the caregivers and family.
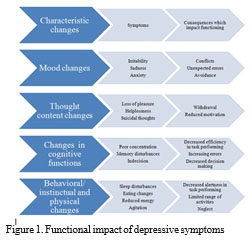
Functional impact of depressive symptoms can be summarized in Figure 1.
Referring to the personal plan, in depression, the daily activities, family relationships and social life.
Specific areas of health: physical, psychological and social. Each of these can be measured either by objective assessments or by subjective perception. In addition each of these areas include several aspects such as different symptoms, ability to function and disability.
While all mood disorders are associated with a lower quality of life, major depressive disorder shows a strong association with the quality of life as a whole and dysthymia and bipolar disorder with social interaction. (Axis I_andQol). (7) The severity of the current episode is one of the most important factors when assessing its social impact. Hence, the number of days that a person with depression has not been able to fulfill her role in the last
365 days increased from 3 in the case of mild depression to 96 in the case of severe depression. (8) Among the persons with major depressive disorder in the past 12 months almost all (96.9%) reported a deterioration in role functioning associated with depression on at least one of the four areas of SDS, 87.4% of them describing the damage as being at least moderate. (9)
In one study which assessed the damage to the quality of life in patients with depressive and anxiety disorders (1) 85% of patients with chronic depression or double depression, only 63% of patients diagnosed with major depressive disorder and only 56% of those diagnosed with dysthymia presented on the quality of life questionnaires scores adequate to the interval of severe degradation.
The same study indicates that specific symptoms of the disease have a modest influence over the quality of life, suggesting the involvement of other factors. Such factors could be the presence of algal symptoms and comorbid disorders, also personality traits, financial resources, availability of social support and achieving personal goals and personal success level.
The association between algal symptoms or some somatic disorders and depression lead to a significant further deterioration in quality of life (10)(11)(12) and influences the results obtained after treatment. The presence of algal symptoms is associated with less improvement in quality of life as perceived by patients following antidepressant treatment (10), and previous history of major depressive disorder is associated with a greater decline in physical functioning and health status mental worse among patients diagnosed with breast cancer. (13). Dissatisfaction / discontent with life on a long term might be a stronger predictor of major depressive disorder compared with concomitant discontent / dissatisfaction who seems to correlate strongly with depressive symptoms. (14)(15)Some aspects of depression may be considered intangible and difficult to measure. These include pain, family’s , caregivers’ and friends’ woe and stress suffered by them and other types of relationships, which, although can not be measured directly, manifest by disruption of Because these negative consequences of depression are
complex and difficult to measure, they are generally not included in the cost estimates of depression, andformal estimations of the cost of depression both the direct and the indirect ones. However, the vast majority of interventions for the treatment of major depressive disorder are considered cost-effective.(16) This should be an additional argument for early detection and proper treatment of mood disorders.
References:
1.Rapaport MH, Clary C., Fayyad R., Endicott J.: Quality-of-Life
Impairment in Depressive and Anxiety DisordersAm J Psychiatry 2005;
162:1171–1178.
2.Centers for Disease Control and Prevention. Measuring Healthy Days. Atlanta, Georgia: CDC, November 2000.
3.World Health Organization.1997 The World Health Organization Quality of Life instruments (The WHOQOL-100 and THE WHOQOL- BREF) WHO/MSA/MNH/PSF/97.4.
4.Daly E.J., Trivedi M.H. et al. Health-related quality of life in depression: A STAR*D report Annals of Clinical Psychiatry
2010;22(1):43-55.
5.Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Geneva, Switzerland;World Health Organization, 1996.
6.Nemeroff C.B., The burden of severe depression: A review of diagnostic and treatment alternatives, Journal of Psychiatric Research (2006), doi:10.1016/j.jpsychires.2006.05.008.
7.Guan B, Deng Y, Cohen P, Chen H. Relative impact of Axis I mental disorders on quality of life among adults in the community. J Affect Disord. 2011;131:293–298.
8.Kenedy S., Gorwood Ph., Successful Management of Major
Depressive Disorder Evolving Medicin Ltd 2012.
9.Kessler, C.R. et al.: The Epidemiology of Major Depressive Disorder Results From the National Comorbidity Survey Replication.(Reprinted) JAMA June 18, 2003 Vol 289, No23, 3095-3105
10.Novick D., Montgomery W. et al: Do concomitant pain symptoms in patients with major depression affect quality of life even when taking into account baseline depression severity? Patient Preference and Adherence
2013:7 463–470.
11.O’Neil A., Stevenson C.E., Williams E.D., Mortimer D., Oldenburg B, Sanderson K. The health-related quality of life burden of co- morbidcardiovascular disease and major depressive disorderin Australia: findings from a population-based,cross-sectional studyQual Life Res (2013) 22:37–44.
12.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Mortality and quality of life 12 months after myocardial infarction: effects of depression and anxiety. Psychosom Med.2001;63(2):221–30.
13.Jim H.S.L., Small B.J., Minton S., Andrykowski M., Jacobsen P.B. History of Major Depressive Disorder Prospectively Predicts Worse Quality of Life in Women with Breast CancerAnn Behav Med. 2012 June
; 43(3): 402–408.
14.Rissanen T., Viinamäki H. et al.: Long term life dissatisfaction and subsequent major depressive disorder and poor mental health. BMC Psychiatry 2011 11:140.
15.Koivumaa-Honkanen H, Kaprio J, Honkanen R, Viinamäki H, Koskenvuo M. Life Satisfaction and depression in a 15-year follow-up of healthy adults. Soc Psychiatry Psychiatr Epidemiol 2004, 39:994-999.
16.Van Steenbergen-Weijenburg, van der Feltz-Cornelis C.M. et al.: Cost-effectiveness of collaborative care for the treatment of major depressive disorder in primary care. A systematic review. BMC Health Services Research 2010 10:19.
***




