A NEW INSTRUMENT FOR ASSESSMENT OF MILD NEUROCOGNITIVE DISORDER
Abstract
Introducere: Evaluarea tulburărilor neurocognitive ușoare este o problemă foarte importantă în cercetare și în practica clinică. Obiectiv: Determinarea eficacității unui nou instrument de evaluare a tulburării neurocognitive ușoare. Metodă : Testul de evaluare a modificărilor psihice ușoare (MIX Test) a fost elaborat în conformitate cu DSM-5 pentru evaluarea tulburarărilor neurocognitive ușoare. Instrumentul conține teste pentru memorie, atenție, funcțiile executive, percepția vizuo-spațială și limbajul ; este nevoie de aproximativ 15 minute pentru administrare. Acesta a fost aplicat la 24 de pacienti diagnosticati cu tulburare neurocognitivă ușoară sau cu alte tulburări psihice cu intensități ale tulburării cognitive comparabile cu tulburările neurocognitive ușoare (schizofrenie-6, post- accident vascular cerebral-6, tulburare neurocognitivă-4, tulburare depresiva majora ușoară, moderată cu intensitatea-4, tulburarea bipolară-2, diabet zaharat-2) și la 30 de martori sănătoși. Subiecții au avut vîrste între 33- 90 ani (medie ~ 55 ani), ≥ 9 ani de educație și scorurile MMSE ≥26. Rezultate : Algoritmul de notare a testului a fost standardizat cu un scor maxim total de 33. Valoarea medie a scorului total a fost de 19,4 (SD 6,8) pentru grupul de risc și 28,4 (SD 2,2) pentru grupul de control. Nu a fost o diferență statistică semnificativă între mediile și distribuțiile scorurilor totale între cele două grupuri. Concluzii : MIX test este capabil să diferențieze între un grup de subiecți normali și un grup de subiecti diagnosticați cu tulburare neurocognitivă ușoară sau cu alte tulburări psihice cunoscute de a prezenta diferite intensități ale tulburărilor cognitive comparabile cu tulburarea neurocognitivă ușoară. Testul este un instrument promițător de evaluare a tulburarărilor neurocognitive ușoare și a disfuncțiilor proceselor cognitive.
INTRODUCTION
Numerous terms and concepts have been used to describe the transitional stage from normal cognitive aging to dementia. The concept of mild cognitive impairment proposed by Petersen in 1997 (1) referred initially exclusively to problems in the domain of memory. However, Petersen et al. (2, 3) later defined several MCI subtypes (amnestic, multiple-domain, and single non- memory domain) that described better the heterogeneous group of mild cognitive deficits.
DSM-5 describes this less severe level of cognitive impairment under the concept of mild neurocognitive disorder (4). Mild neurocognitive disorder (NCD) exists as a spectrum of cognitive and f u n c t i o n a l i m p a i r m e n t t o g e t h e r w i t h m a j o r neurocognitive disorder (formerly called dementia in DSM-IV).
The diagnostic features of mild NCD in DSM-5 are: modest cognitive decline from a previous level of performance in one or more cognitive domains, based on
1: concern of the individual informant, or clinician and 2: a modest impairment in cognitive performance, preferably documented by standardized neuropsychological testing. As additional criteria, cognitive deficits are not better explained by another mental disorder and are not accompanied by dependence in activities of daily living. There are numerous etiologies responsible for mild NCD: Alzheimer’s disease, frontotemporal lobar degeneration, Lewy body disease, vascular disease, traumatic brain injury, substance/medication use, HIV infection, prion disease, Parkinson’s disease, Huntington’s disease, other medical conditions (4).
DSM-5 gives also a detailed presentation of cognitive processes from each cognitive domain, with examples of symptoms or observations and specific assessments. There are six cognitive domains: complex attention, executive function, learning and memory, language, perceptual-motor and social cognition. Cognitive domains cover several cognitive processes, that represents the components of the cognitive functioning in a particular area. By example, learning and memory domain covers the following cognitive processes: immediate memory, recent memory, very-long-term memory and procedural learning. Each cognitive domain can present a non homogenous impairment of specific cognitive processes, according to etiology and to the stage of mild or major NCD. Therefore, choosing the cognitive processes and the appropriate difficulty level of assessment are important issues in the construction of a test for assessment of mild NCD.
Neuropsychological assessment is one of the methods to assess the cognitive decline, in addition to history of cognitive complaints. DSM-5 defines the cut- offs of neuropsychological test performances: mild NCD between 1st and 2nd standard deviation and major NCD
below the 2nd standard deviation of the assessments (4).
Anyway, brief instruments for assessment of mild neurocognitive disorder suitable for assessment of corresponding impaired cognitive processes and using the cut-offs described in DSM-5 are also still lacking.
MATERIALS AND METHODS Test development
We developed a pencil and paper test battery for assessment of mild NCD starting from the cognitive domains described in DSM-5. For the construction of the test, we selected the cognitive domains of attention, memory, executive functions, language and perceptual- motor. We did not selected social cognition because this type of impairment is less encountered and assessments of this domain are more time consuming. For each cognitive domain several cognitive processes, corresponding assessments and scoring algorithm were selected by one of the authors (MVZ) based on and several criteria: impairment of cognitive processes is specific to mild NCD, ability of assessments to predict conversion to major NCD, difficulty level of assessment suited for mild NCD and short duration of administration. The authors used a scoring algorithm aimed to reflect DSM-5 conceptualization of three levels of cognitive functioning: normal, mild NCD and major NCD. The purpose of the test was to represent a short battery for screening of mild NCD and also for assessing cognitive processes impaired in mild NCD. The test was named Mild Mental Changes Assessment Test (MIX Test).
The following assessments were selected for the construction of this test battery, based on previous data in the literature regarding neuropsychological assessments diagnostic for mild NCD (5-10):
-memory:
12 words list learning, 3 early recalls, one delayed recall; The administration speed was 1word/1,5s; each
administration was followed by an early recall trial of 30s.
There were three consecutive learning-early recall trials;
10 minutes after the last learning trial a delayed recall trial of 60s was administered. We calculated 2 scores: total early recall for the 3 trials (total correct early recall items minus total early recall intrusions) and total delayed recall (correct delayed recall items minus delayed recall intrusions). We did not counted repetitions (neither correct repetitions nor repetitions of intrusions). The 12 words included in the list were: chair, rabbit, prune, screwdriver, ballerina, T-shirt, building, lake, mathematics, gold, tomato, ant.
-attention:
s y m b o l – d i g i t s u b s t i t u t i o n – n u m b e r o f c o r r e c t substitutions during 1 minute (9 symbol-digit pairs on top of page (Figure 1), substitution lines with 15 symbols/line, 5 items for one trial at the beginning of the assessment); patients made the substitutions orally; we chose oral modality of administration because it allows to test for patients with sequelae of stroke;
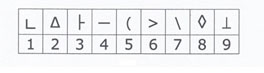
Figure 1. Symbol-digit pairs used in digit symbol substitution task
-executive functions:
flexibility: category and letter verbal fluency; animals for
1minute, words starting with letter F for 1min, scoring of correct nouns, diminutives or proper nouns are not allowed;
inhibition: conflicting instructions; patient taps once when examiner taps twice and twice when examiner taps once, examiner taping sequence: 112212221121;
working memory: digit span backward; 3 and 4 digits sequences administered in ascending order length, maximum 2 trials for each number of digits, speed of administration one digit/second; maximum correct number of digits was recorded;
similarities test – number of correct abstract similarities (apple-orange, bicycle-train, watch-scale, laugh- sadness);
clock drawing (11:10) – hands positioning;
-visuo-motor abilities:
cube copying (copying a sample item on the same sheet);
clock drawing (11:10) – numbers positioning;
-language:
confrontation naming: 22 drawings of objects encountered with low to high frequency (Figure 2); we counted naming errors
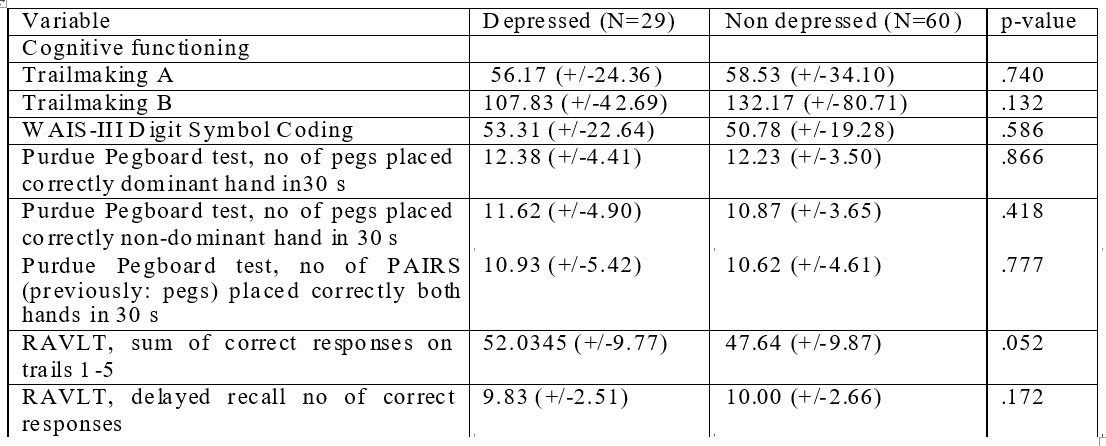
Figure 2. Pictures used for confrontation naming
Patients
MIX test was applied to 24 patients diagnosed with mild neurocognitive disorder or with other disorders known to present with intensities of cognitive impairment c o m p a r a b l e t o m i l d n e u r o c o g n i t i v e d i s o r d e r : schizophrenia – 6, post-stroke – 6, mild NCD – 4, major depressive disorder of moderate intensity – 4, bipolar disorder – 2, diabetes mellitus – 2; and to 30 healthy controls (with no condition known to present with high risk for cognitive impairment). We will refer to the first group as “group at risk” because in this group predominate patients diagnosed with disorders that present high prevalences of cognitive impairment at intensities comparable to mild neurocognitive disorder, but not formally diagnosed with cognitive impairment.
Patients were selected between June and November 2013 from Obregia Clinical Psychiatry Hospital – Bucharest and Ana Aslan National Institute of Gerontology and Geriatrics – Bucharest. We excluded subjects with MMSE<26, ≤8years of education or unable to do the test due to sensorial or motor impairments. All patients in the group at risk (except patients with major depressive disorder) were chronic and stable. For diagnosis of mental disorders DSM-5 criteria were used. The study had approval of the ethics councils of the two institutions and the subjects gave written consent.
Statistics
To compare scores of the two groups we used T test for independent samples for means comparison and Mann-Whitney test for distributions comparison. To test for normal distribution of data we used Shapiro-Wilk Test of Normality.
RESULTS
Subjects in the two groups were similar regarding age, education and sex ratio. The mean age was
58 years in the group at risk and 55 years in the control group. There was a predominance of female subjects (66% in the control group and 58% in the groups at risk). Subjects had an average education of 12,3 years in control group and 13,2 years in the control group. All subjects were speaking Romanian as primary language.
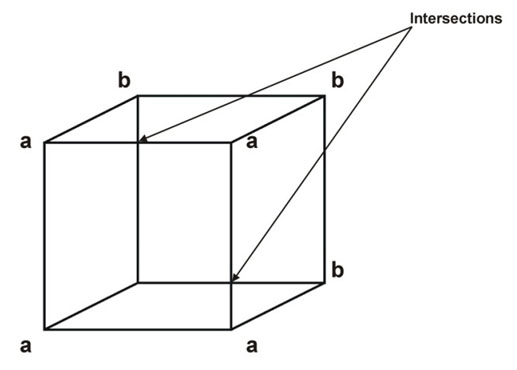
Figure 3. Cube copying. The two intersections and squares aaaa and bbbb are one of the items used for interpretation.
MIX test scoring algorithm
Each of the domains of memory, attention, visuo- motor abilities and language were granted 6 points and executive functions 9 points (due to higher number of cognitive processes involved in executive functions). Results were scored categorically for sentence repetition and inhibition (1: correct, 0: incorrect). Space and time orientation, digit span backward, clock drawing – hands positioning, clock drawing – numbers positioning and cube copying (Figure 3) were scored based on predetermined algorithms (Tabel 1).
For the other assessments we obtained raw scores such as described in the Materials and Methods section of the article. We then used raw scores to develop a scoring algorithm based on the mean and standard deviation of each task of the control group. As a general rule, we followed DSM-5 recommendations regarding the cut-off of 1-2SD for mild NCD and <2SD for major NCD.
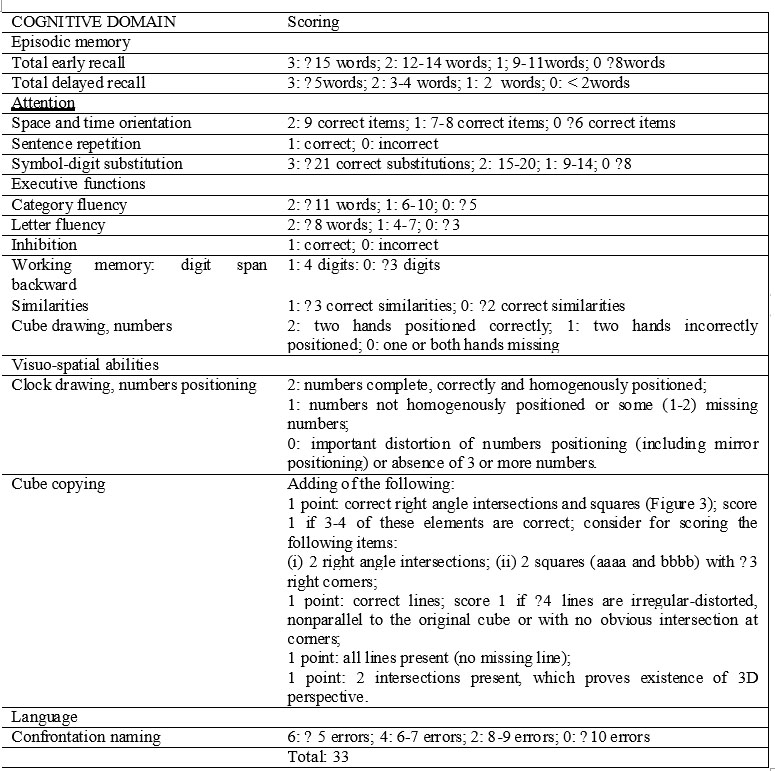
Table 1. MIX Test scoring algorithm
To be able to use mean and standard deviation of raw scores from the control group, one need to assume normal distribution of these data. In order to test for normal distribution of data in the control group, we used Shapiro-Wilk Test of Normality, a test that calculates how much data significantly deviate from a normal distribution; if p<0.05 data are not normally distributed, if p>0,05 we can assume normal distribution. We found in control group p>0,05 for total early recall, total delayed recall, digit-symbol substitution, category fluency and letter fluency, so we assumed normal distribution for these data and used the mean and the standard deviation of each task to develop a scoring algorithm. For confrontation naming errors we found a non-normal (p<0.05) left- skewed distribution in control group; after natural logarithm transformation of confrontation naming data, we found p>0,05 at Shapiro-Wilk test, so we assumed a normal distribution for the transformed data. We used mean and standard deviation of transformed data to develop a scoring algorithm for confrontation naming.
The final structure and scoring of MIX test are presented in Table 1. The minimum score is 0 and the maximum is 33.
We then calculated total scores of MIX and obtained a mean of 29,44 in control subjects (SD=2,29) and 20,25 (SD=7,01) for subjects in the group at risk. To compare means and distributions of the two groups we used T test for independent samples and Mann-Whitney test and found a significant statistical difference for both tests (p<0,01).
DISCUSSION
In the present study, we developed a test for assessment of cognitive impairment which is suitable for use in patients with mild neurocognitive disorder. The tasks that constitute the test cover 5 cognitive
domains: memory, attention, executive functions, visuo- spatial perception and language.
We showed that MIX test is able to differentiate between a group of normal subjects and a group of subjects diagnosed with mild neurocognitive disorder or with other disorders known to present with intensities of cognitive impairment comparable to mild neurocognitive disorder. Although we did not include in the group at risk only patients with proven mild NCD because of small number of such patients in the settings were the study took place, the high prevalence of cognitive impairment at a level of impairment comparable to mild NCD represents an useful surrogate for the population of mild NCD patients. In addition we excluded from the study subjects with MMSE scores < 26, which significantly reduces the risk to include patients with dementia in the group of patients at risk of cognitive impairment. Although we did not use a gold standard for assessment of cognition, the presumed high prevalence of cognitive impairment in the group at risk might compensate for this methodological issue. To establish the diagnostic performance of MIX test, a comparison with a gold standard is needed in future studies.
The test has a wide representation of cognitive processes in five cognitive domains: memory, attention, executive functions, visuo-spatial perception and language, and assessments are constructed for a level of impairment specific to mild NCD. The broad coverage of cognitive processes make the test suitable for use in a variety of disorders associated with a mild level of cognitive impairment. There is an important presence of executive function processes in the MIX test, which make it suitable for patients with mild vascular cognitive impairment, as recommended by guidelines (5). The broad representation of cognitive processes makes also the test suitable for assessments of other disorders that produce mild NCD. However, a future discriminative analysis is needed to establish the presumed correspondence between assessments and cognitive processes. The low number of subjects in the control group and the heterogeneity of subjects in the group at risk are not appropriate for such analysis.
The brevity of administration (about 15 minutes) make the test useful for screening of mild NCD in clinical practice. The tasks composing the test have proven to be predictive of conversion of mild NCD to major NCD (delayed recognition (8, 9), processing speed (8), executive functions (8,10)) which might make the test a useful instrument for prognosis.
Similar instruments for screening of mild NCD exists in use. MOCA (11) is a briefer instrument (10 minutes), but has a lower representation of executive functions in comparison to MIX. Also, in comparison to MoCA, MIX contains tasks that proved to be predictive for conversion to major NCD: 12 memory list with 3 learning trials and one delayed recall, and a symbol-digit substitution test. ACE-R (12) and DemTECT (13) are also useful instruments to screen for mild NCD, but they have been developed for screening of dementia and hence the level of difficulty is not best suited for mild NCD. Other screening instruments for mild NCD contains few cognitive processes assessments -ABCS (14), Chinese Abbreviated Mild Cognitive Impairment Test (15), M@T (16), Montpellier screen (17)- or take too much time for administration -FMLL mini-battery (18), CAB (19). MIX test might present some advantages, because it covers a large number of cognitive processes, contains tasks proved to be predictive of conversion to major NCD and its administration is quite short.
CONCLUSION
In conclusion, MIX test is able to differentiate between two groups of normal subjects and patients at risk for cognitive impairment. The test is a promising tool for assessment of mild neurocognitive disorder and of specific impaired cognitive processes. Future studies are needed to establish the diagnostic and psychometric performances of the test.
ACKNOWLEDGEMENT: This paper is supported by the Sectoral Operational Programme Human Resources Development (SOP HRD) 2007-2013, financed from the European Social Fund and by the Romanian Government under the contract number POSDRU/107/1.5/S/82839.
ABBREVIATIONS:
NCD: neurocognitive disorder
REFERENCES
1.Petersen RC, Smith GE, Waring SC et al. Aging, memory, and mild cognitive impairment. Int Psychogeriat 1997;9(1): 65-9.
2.Petersen RC, Doody R, Kurz A et al. Current concepts in mild cognitive impairment. Arch Neurol 2001;58(12): 1985-92.
3.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med 2004;256(3): 183-94.
4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013, 591-644.
5.Hachinski V, Iadecola C, Petersen RC et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke 2006;37(9): 2220-41.
6.Libon DJ, Xie SX, Eppig J at al. The heterogeneity of mild cognitive impairment: a neuropsychological analysis. J Int Neuropsychol Soc 2010;16(1): 84-93.
7 . L e h r n e r J , M a l y J , G l e i s s A , A u ff E , D a l – B i a n c o P. Neuropsychological performance and mild cognitive impairment subtypes in patients reporting cognitive problems attending a memory outpatient clinic. Euro J Ger 2008;10(2): 1-10.
8.Chapman RM, Mapstone M, McCrary JW et al. Predicting conversion from mild cognitive impairment to Alzheimer’s disease using neuropsychological tests and multivariate methods. J Clin Exp Neuropsychol 2011;33(2): 187-99.
9.Guo Q, Zhao Q, Chen M, Ding D, Hong Z. A comparison study of mild cognitive impairment with 3 memory tests among Chinese individuals. Alzheimer Dis Assoc Disord 2009; 23(3): 253-9.
10.Ingles JL, Wentzel C, Fisk JD, Rockwood K. Neuropsychological predictors of incident dementia in patients with vascular cognitive impairment, without dementia. Stroke 2002;33(8): 1999-2002.
11.Nasreddine ZS, Phillips NA, Bédirian V et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53(4): 695-9.
12.Mioshi E, Dawson K, Mitchell J, Arnold R, Hodges JR. The Addenbrooke’s Cognitive Examination Revised (ACE-R): a brief cognitive test battery for dementia screening. Int J Geriatr Psychiatry
2006;21(11): 1078-85.
13.Kalbe E, Kessler J, Calabrese P et al. DemTect: a new, sensitive cognitive screening test to support the diagnosis of mild cognitive impairment and early dementia. Int J Geriatr Psychiatry 2004;19(2): 136-43.
14.Molloy DW, Standish TI, Lewis DL. Screening for mild cognitive impairment: comparing the SMMSE and the ABCS. Can J Psychiatry 2005;50(1): 52-8.
15.Lam LC, Tam CW, Lui VW et al. Screening of mild cognitive impairment in Chinese older adults – a multistage validation of the C h i n e s e a b b r e v i a t e d m i l d c o g n i t i v e i m p a i r m e n t t e s t . Neuroepidemiology 2008;30(1): 6-12.
16.Rami L, Molinuevo JL, Sanchez-Valle R, Bosch B, Villar A. Screening for amnestic mild cognitive impairment and early Alzheimer’s disease with MAT (Memory Alteration Test) in the primary care population. Int J Geriatr Psychiatry 2007;22(4): 294-304.
17.Artero S, Ritchie K. The detection of mild cognitive impairment in the general practice setting. Aging Ment Health 2003;7(4): 251-8.
18.Abizanda P, López-Ramos B, Romero L et al. Differentiation between mild cognitive impairment and Alzheimer’s disease using the FMLL mini-battery. Dement Geriatr Cogn Disord 2009;28(2): 179-86.
19.Nordlund A, Påhlsson L, Holmberg C, Lind K, Wallin A. The Cognitive Assessment Battery (CAB): a rapid test of cognitive domains. Int Psychogeriatr 2011;23(7): 1144-51.
***




