THE ASSESSMENT OF GLOBAL FUNCTIONING IN BIPOLAR PATIENTS WITH COGNITIVE DEFICITS
Abstract
Cursul sever al tulburarii afective bipolare este asociat cu deficite cognitive in domenii ca memoria verbala, memoria de lucru, viteza psihomotorie, fluenta verbala, atentia si viteza de procesare a informatiilor, functia executiva/motivatia si rezolvarea de probleme precum si cu functionalitatea socio-ocupationala scazuta de-a lungul timpului. (1, 2, 3, 4) Nu putem incheia discutia despre aspectele clinico-evolutive ale tulburarii afective bipolare fara sa mentionam rezultatele obtinute intr-un studiu realizat pe 137 pacienti bipolari, in cadrul caruia am evaluat functia cognitiva, functionalitatea si statusul socio-ocupational al acestora.
Acknowledgements:
Prof. Dr. Richard Keefe has approved the free licensee for this research. Duke University holds the copyright for the Brief Assessment of Cognition in Schizophrenia, and it is licensed through NeuroCog Trials, Inc.
Method:
137 bipolar patients met the inclusion criteria (depressive episode: DSM-IV-TR criteria for Major Depressive Episode, HAMD score>=17; manic/hypomanic episode: DSM-IV-TR criteria for Manic/Hypomanic Episode, YMRS score>=12, euthymic: 6month of remission, HAMDscore<=8, YMRSscore<=6; mixed: DSM-IV-TR criteria for Mixed Episode, HAMDscore>8 and YMRSscore>6) and were therefore enrolled in the study. P a t i e n t s w e r e f r e e o f p s y c h o t i c s y m p t o m s (hallucinations/delusions) at the moment of testing. Control group consisted of 62 healthy subjects without history of neurological and/or psychiatric disorder. Cognitive battery (BACS- Brief Assessment of Cognition in Schizophrenia) (5) has been applied in order to assess verbal memory, working memory, psychomotor speed, verbal fluency, attention and speed of information processing, executive function. GAF (Global Assessment Functioning Scale) (6) scale has been applied in order to assess functionality. Following data were collected: demographics, psychiatric history, age of illness onset; c u r r e n t a n d p r e v i o u s t r e a t m e n t ( i n c l u d i n g hospitalizations). Global functioning and socio- occupational status were analyzed in bipolar patients with cognitive deficits.
Results and discutions:
This observational study included 2 groups of subjects: the bipolar group – with 137 patients with Bipolar Disorder, and the control group – with 62 healthy subjects. Socio-demographic characteristics of the samples are presented in Table 1.There were no significant differences between the two study groups regarding age (t = -0.51; 95%CI: [-2.81; 1.66]; p = 0,613), gender and education level (t = 1.09; 95%CI [-0.32; 1.09]; p =0,164).
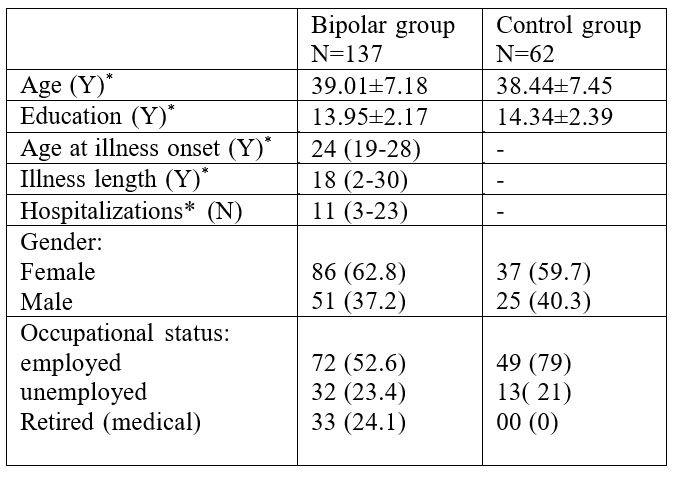
Table 1: Socio-demographic and illness characteristics of the study groups
Y=years; N=numbers; * Values are presented as mean± standard deviation for parametric scale variables and mean (range) for nonparametric scale variables
The bipolar group consists of four subgroups: 54 manic patients, 32 depressive patients, 30 euthymic patients and 21 patients with mixed episodes. Socio-demographic characteristics of the subgroups are presented in Table 2 and illness characteristics of the study subgroups are presented in Table 3.
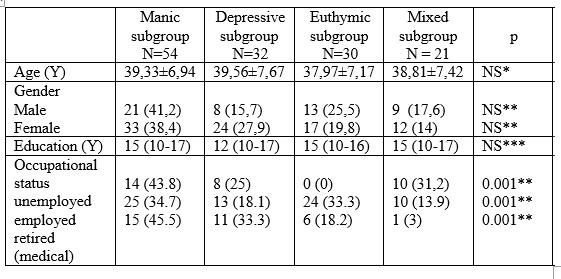
Table 2: Socio-demographic characteristics of study subgroups
Y= Years; Values are presented as mean±s.d for continuous parametric data, median (range) for continuous nonparametric data and absolute number (percent) for categorical data; * ANOVA; ** chi-square test;
***Kruskal-Wallis test; NS: no statistical significant (p ≥0.05
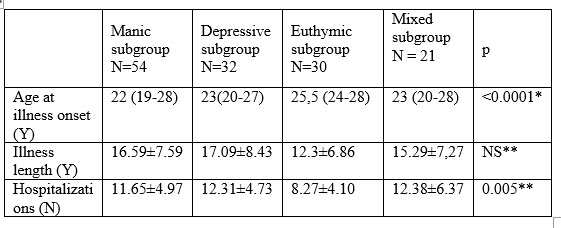
Table 3: Illness characteristics of the study subgroups Y=years; N=numbers; Values are presented as mean±s.d for continuous parametric data, median (range) for continuous nonparametric data; *
Kruskal-Wallis test; ** ANOVA; NS: no statistical significant (p ≥0.05)
The previous episodes’ polarity, in the study subgroups, is shown in Chart 1, and we may notice a predominance of manic episodes in the patient’s medical history. In concordance with the previous studies showed in the literature (7) this study highlights the fact that the existence of previous manic episodes deteriorates the cognitive function more than the existence of previous mainly depressive episodes. But we did not notice significant differences between GAF scores in patients with previous mainly manic episodes and previous mainly depressive episodes.
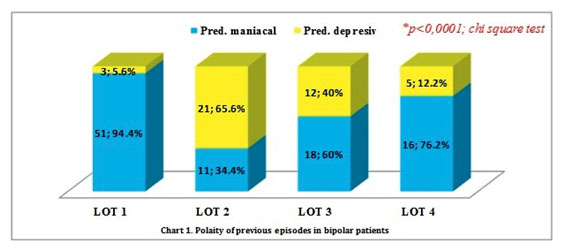
Pred. Manic = predominantly manic episodes, Pred. Depressive = predominantly depressive episodes
At the level of the entire group of bipolar patients, the categories of GAF (Global Assessment Functioning scale) scores have shown a similar statistical distribution [GAF 41-50: 52 cases; 38% vs. GAF 51-60: 49 cases; 35.8% vs. GAF 61-70: 36 cases; 26.3%; p = 0.205].
After adjusting on the current episode type, there were highlighted statistically significant differences between categories of GAF scores and the 4 subgroups of bipolar patients as follows: while for most patients of Group 1 (24 cases; 44.4%) and Group 4 (13 cases; 61.9%) the GAF scores were included in the category of 41-50 points, for the majority of patience in Group 2 (17 cases; 53.1%) the GAF scores were contained within the category 51-60 points, and for most patients of Group 3 (22 cases; 73.3%) the GAF scores were comprised in the category 61-70 points (Chart 2).
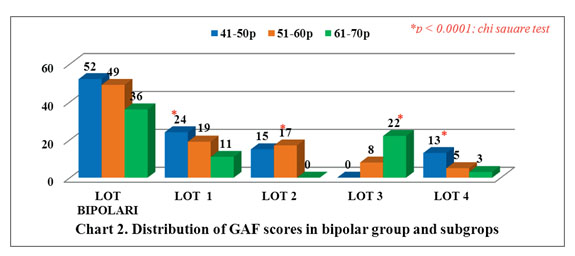
GAF score 40-50 (any serious deterioration in social, occupational, school functioning – e.g.: no friends, unable to keep a job, cannot work); GAF score 51-60 (moderate difficulty in social, occupational, school functioning – e.g.: few friends, conflicts with other people or with coworkers); GAF score 61-70 (some difficulty in social, occupational, school functioning – e.g. occasional truancy, household theft, but generally fairly good functioning, has some meaningful interpersonal relationships).
At the level of the entire group of bipolar patients, the bivariate correlation analysis has revealed a directly proportional statistically significant association between the categories of GAF score and the patients’ age at illness onset [r = 0.474; r 2 = 0.225; p < 0.0001]. Also, at the level of the entire group of bipolar patients, there has been evidenced an indirectly proportional statistically significant association between the categories of GAF score and the illness duration of these patients [rs = -0.443; r 2 = 0.196; p < 0.0001]. Similarly, the number of s
hospitalizations was significantly statistically correlated with the GAF score categories at the entire group’s level [rs = -0.594; r 2 = 0.353; p < 0.0001].
About half of the bipolar group’s patients are not included in the work field, being unemployed or medically retired. When analyzing the subgroups, it has been observed that manic patients and those with mixed episodes have similar employment percentages, but less than 50%, and the lowest employment percentage is obtained by patients in depressive episodes (40%). The rate of non-entering employment and disability among bipolar individuals is significantly higher than for the normal population (8, 9). A previous review which has brought together the results of several studies has concluded that 57-65% of patients with bipolar affective disorder are not employees (compared to 6% in the general population) (10). The percentages obtained in this thesis are close to those in the literature, namely: manics 53.7%, patients with depressive episodes 59.4%, and patients with euthymic episodes 52.4%.
Among the functionality predictors, which were the most common in previous studies, we mention the depressive symptoms and the cognitive impairment (9, 10, 11), our research being in accordance with these data. The group of bipolar patients has shown cognitive deficits in all assessed cognitive domains, compared to the healthy group. At the subgroups analysis, manic patients showed the most pronounced cognitive deficits, compared with other subgroups. These cognitive deficits persist in the euthymic period too.
The studies of Martinez-Aran et al. (12), Wingo et al. (13), Bonnin et al. (14) and Tabares-Seisdedos et al. (15), are recognized, being studies in which they support the cognitive impairment’s negative implications for the overall functioning. In concordance with the previous study, we found in the bipolar group GAF scores directly correlated to the scores obtained in all cognitive domains under assessment. Despite high energy, the impaired cognitive function does not support performance and the final result is an important decrease of functionality. Although patients with depressive episodes had the lowest occupational status, the lowest overall functionality was recorded, in this study, for patients with manic and mixed episodes (patients with the lowest scores regarding the assessment of verbal memory, working memory and executive function/judgement and problem solving). Most patients with manic and mixed episodes were included within the GAF score 40-50, while the majority of depressed patients obtained a GAF score of 51-60. Depressed patients, associated with the lowest occupational status, have the largest deficits in the cognitive domains of verbal fluency and psychomotor speed. Even if most euthymic patients were included within GAF 61-70, in terms of overall functionality, however, none of these patients exceeded this GAF range. These periods of clinical remission (euthymia) are marked b y s u b t l e s o c i a l , o c c u p a t i o n a l , a n d c o g n i t i v e dysfunctions, as stated by Lima et al. (16).
The disease’s long length, the large number of psychiatric hospitalizations and early onset of the illness were directly correlated to low scores of overall functioning, being able to conclude, with the help of this study’s results, that a severe course of the bipolar disorder is related to the low overall functionality. These conclusions are consistent with what Burdick and his collaborators presented, namely: a severe evolution of the disease (defined by an increased number of hospitalizations) is a significant and independent predictor of occupational damage regarding p a t i e n t s w i t h b i p o l a r a ff e c t i v e d i s o r d e r ( 1 7 ) . Hospitalizations are not only signs of disease severity but also interruptions of the personal functioning and development, discontinuities of personal evolution and a stigma motive in society.
What are the clinical implications of the fact that, for many patients, functional recovery cannot be expected to occur along with the achievement of syndrome or symptomatic recovery? Patients at high risk of failing to achieve functional recovery seem to be those who have recurrent, more severe and prolonged acute episodes. Rush states that for these patients there should be a special stage in which to try to identify and effectively treat the relevant cause of incomplete functional recovery, in order to normalize the daily functioning (18).
Conclusions:
Patients with bipolar disorder and cognitive deficits show impairment of global functioning and lower socio- occupational status.
References
1.Zubieta JK, Huguelet P, O’Neil RL et al. Cognitive function in euthymic bipolar I disorder. Psychiatry Res. 2001;102(1):9-20. Levy
2.B. Illness severity, trait anxiety, cognitive impairment and heart rate variability in bipolar disorder. Psychiatry Res. 2014 Dec 30;220(3):890- 5.
3.Elshahawi HH, Essawi H, Rabie MA, Mansour M, Beshry ZA, Mansour AN. Cognitive functions among euthymic bipolar I patients after a single manic episode versus recurrent episodes. J Affect Disord. 2011;130(1-2):180-191.
4.Spollen JJ. Impaired Cognition in Bipolar Disorder: Something to Think About. http://www.medscape.org/viewarticle/457153 Accesat pe 3 August 2015.
5 . N e u r o C o g Tr i a l s . L i c e n s e d i n s t r u m e n t s . Av a i l a b l e a t : www.neurocogtrials.com/licensed-instruments.
Accessed April 2, 2012
6.Endicott J, Spitzer RL, Fleiss JL et al. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766-771.
7.Goldberg JF, Burdick KE. Cognitive dysfunction in bipolar disorder. A guide for clinicians. Washington, DC, USA: American Psychiatric Press 2008
8.Kogan JN, Otto MW, Bauer MS et al. Demographic and diagnostic characteristics of the first 1000 patients enrolled in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Bipolar Disord. 2004:6:460-469.
9.Deckersbach T, Nierenberg AA, Kessler R et al. Cognitive rehabilitation for bipolar disorder: An open trial for employed patients with residual depressive symptoms. CNS Neuroscience and Therapeutics. 2010;16:298-307.
10.Huxley N, Baldessarini RJ. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9:183-196.
11.Merikangas KR, Ames M, Cui L et al. The impact of comorbidity of mental and physical conditions on role disability in the US adult household population. Arch Gen Psychiatry. 2007;64:1180-1188.
12.Martinez-Aran A, Vieta E, Colom F et al. Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord. 2004a;6:224-232.
13.Wingo AP, Harvey PD, Baldessarini RJ. Neurocognitive impairment in bipolar disorder patients: functional implications. Bipolar Disord. 2009;11(2):113–125.
14.Bonnin CM, Martinez-Aran A, Torrent C et al. Clinical and neurocognitive predictors of functional outcome in bipolar euthymic patients: a long-term, follow-up study. J Affect Disord. 2010;121(1- 2):156-60.
15.Tabares-Seisdedos R, Balanza-Martiney V, Sanchez-Moreno J et al. Neurocognitive and clinical predictors of functional outcome in patients with schizophrenia and bipolar I disorder at one-year follow-up. J Affect Disord. 2008;3(109):286-299.
16.Lima FM, Czepielewski LS, Gama CS et al. Cognitive and psychosocial impairment in remitted bipolar patients. Psicodebate. 2014;14(2):25–38.
17.Burdick KE, Goldberg JF, Harrow M. Neurocognitive dysfunction and psychosocial outcome in patients with bipolar disorder at 15-year follow-up. Acta Psychiatr Scand. 2010;122(6):499-506.
18.Rush AJ, Trivedi MH, Wisniewski SR. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905-17.
***




