DIAGNOSTIC CHALLENGES OF A PSYCHOTIC DISORDER IN A PATIENT WITH LIVER TRANSPLANT
Abstract
We present the case of a 39 year-old woman who underwent liver transplantation in 2011 at Fundeni Clinical Institution and who developed an acute psychotic episode, with psychomotor agitation, persecutory delusion, visual and auditory hallucinations, psychotic anxiety and sleep problems 3 days after the transplant, treated with Olanzapine. The patient was admitted to the psychiatric emergency unit of Clinical Hospital of Psychiatry “Prof. Dr. Al. Obregia” in August 2014 for a second psychotic episode, 6 months after Olanzapine withdrawal. Having difficulties in establishing a certitude diagnosis, we considered many differential diagnoses including postoperative delirium, steroid induced psychosis and schizophrenia. CONCLUSIONS: Similar to other populations with chronic physical illnesses, patients with organ transplant are at elevated risk for psychiatric symptoms and diagnosable psychiatric disorders. Mood and anxiety- related disorders are the most common psychiatric illnesses observed both pre- and post transplant, although acute cognitive impairment and delirium are often seen shortly pre transplant and preoperatively due to metabolic perturbations and the effects of surgery. Psychosis in transplant populations, although rare, is a significant concern because of its potential impact on health and well- being if not carefully managed. Psychiatric complications of liver transplant can manifest in different ways and at various time points which makes detection and management challenging. Given the impact these have on patient and transplant outcome, we stress the importance of vigilance, timely, adequate intervention and of a multidisciplinary approach of patients with liver transplant.
BACKGROUND:
The prevalence of neuropsychiatric complications in liver transplant patients ranges from 8.3% to 64.5% [1,2,3,4,5]. Such complications include delirium, brief psychotic disorder, major depression, mania, adjustment disorder, anxiety and post-traumatic stress disorder, seizures, cerebrovascular disorders, insomnia, migraine, vertigo, movement disorders and peripheral neuropathy [1,2,3]. Psychosis, including conditions such as schizophrenia, schizoaffective disorder, mania, and psychotic depression, is rare in transplant recipients. Moreover, psychosis emerging beyond the postoperative recovery period (and which can therefore not be ascribed exclusively to acute metabolic perturbations associated with surgery and marked medication changes) appears to occur almost exclusively in individuals with pre- transplant histories of such illness. In fact, individuals with a history of psychosis are at high risk for posttransplant recurrences. These patients can do well posttransplant if good social supports, adherence to medical and psychiatric directives, and good control of psychotic symptoms are established prior to transplant. Under these circumstances these patients do not have rates of no adherence that differ from other transplant recipients. The potential for good management post transplant, plus the very negative effects if psychoses are not well managed, make them important conditions to consider during the pretransplant assessment. Despite common beliefs, it is not clear that a prior psychiatric history makes a patient more susceptible to the potential of immunosuppressive medications, especially steroids, to produce or exacerbate psychotic symptoms or mania (i.e. “steroid psychosis”). The appropriate use of antipsychotic medication is usually adequate to prevent or manage these symptoms if they emerge, and care must be taken that these medications are not discontinued in the early post transplant phase [6,7].
We present a case of a 39 year-old woman who underwent liver transplantation for decompensated (both vascular and parenchyma) autoimmune hepatic cirrhosis (MELD score=13 with liver failure) in 2011.
The patient was admitted to the psychiatric emergency unit of Clinical Hospital of Psychiatry ”Prof. Dr. Al. Obregia” in August 2014 for: psychomotor agitation, imperative and commendatory auditory hallucinations, psychotic anxiety and sleep disorders. These symptoms occurred during hospitalization at Fundeni Clinical Institution in Bucharest, where she was admitted on July 30 2014 for marked fatigability, fever and jaundice. On August 12 2014 she was transferred to our emergency unit because she developed hallucinations, delusions and psychomotor agitation.
HISTORY: The patient underwent the liver transplant at Fundeni Clinical Institution where she was admitted between 16.11.2011-01.03.2012. Post-transplant she was administered immunosuppressive treatment with Solu- Medrol, Mycophenolate Mofetil and then Tacrolimus. The secondary diagnoses were: portal vein thrombosis, biliary fistula, Pseudomonas Aeruginosa infection and psychomotor agitation.
During the admission for transplant surgery at Fundeni Clinical Institution in 2011, only 3 days after the liver transplant the patient developed an acute psychotic episode, with psychomotor agitation, persecutory delusion, visual and auditory hallucinations, psychotic anxiety and sleep problems. She was consulted by a psychiatrist who decided to start the treatment with Olanzapine 10 mg/day. After the psychotic episode, Tacrolimus was changed with Sirolimus which was administered for another 4 months then replaced with Cyclosporine because of its well known neurological effects, the patient also developing a biliary fistula during Sirolimus treatment. The patient was very well responsive to the antipsychotic treatment, so she was under Olanzapine between 2011 and 2013, when the treatment was discontinued at the advice of her doctor because patient’s evolution was favorable and she could return to her work as a nurse. For 6 months after discontinuation she had a good functioning until August 2014 when she suffered the second psychotic episode, described above. The patient is married, has a 12 years old child and works as a nurse. She denies the consumption of nicotine, alcohol and caffeine. Her family history is relevant, her mother being diagnosed with schizophrenia. The patient had no personal psychiatric antecedents before her first psychotic episode occurred in 2011, 3 days after liver transplantation. Also, the personal history for other organic diseases was negative.
PSYCHIATRIC EXAMINATION: performed on August
12 2014 revealed a conscious and co operant patient, oriented in time and space, autopsychic and allopsychic oriented, visual and psychic contact easily to start and maintain, psychomotor agitation, expansive mimic and gesture, expressive facies, bizarre behavior (she sits on the back of the chair).
The patient presents imperative and commendatory auditory hallucinations (“I heard a song before and now”, “I’ve heard many voices”, “I don’t know what to think a n y m o r e ” ) , g l o b a l h y p o p r o s e x i a , n o m e m o r y disturbances, accelerated flow and rhythm of thoughts, persecutory delusions (“They keep following me”), expansive mood, psychotic anxiety, disinhibition (“the voices tell me that if I don’t sleep with my doctor I won’t get better”), insomnia, decreased appetite and impaired insight.
SOMATIC EXAMINATION: multiple ecchymoses on the arms, back and belly, post-operative scar on the abdomen, elevated blood pressure (170/110 mmHg), tremor of the arms and elevated pulse (110 bpm) without any other pathological signs.
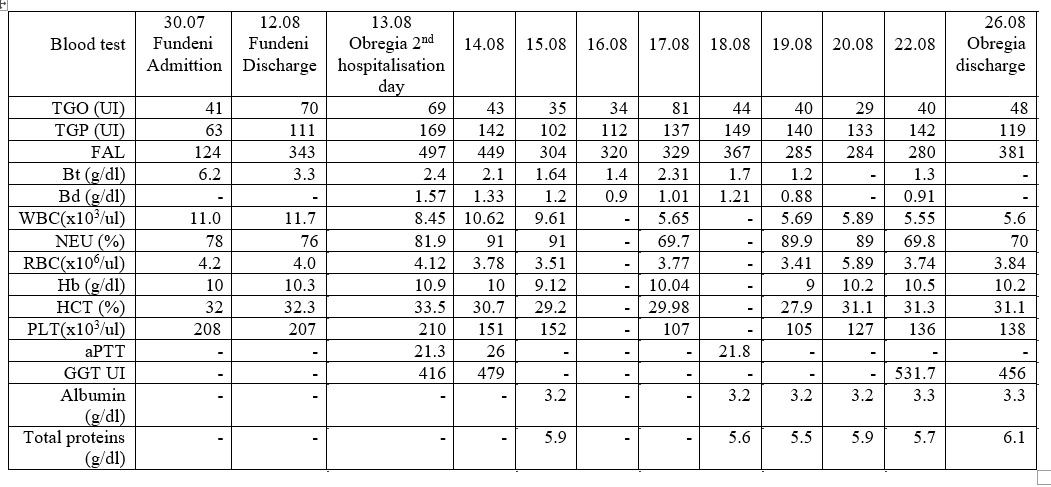
PARA CLINICAL EXAMINATION: Native brain CT was normal. The evolution of the blood tests results (only abnormal parameters extracted) from Fundeni Institute (admission and discharge days) and during hospitalization in Alexandru Obregia Hospital are presented in Table 1. COURSE AND TREATMENT: After admission on
12.08.2014 we initiated treatment with: Diazepam 10 mg,
3 tablets/day, Olanzapine 10 mg/day and Zopiclone 7.5 mg 1 tablet/day. At the recommendation of the gastroenterologist, the psychiatric treatment was completed with: Medrol 4 mg/day, Silivit F 1 tablet/ day, Omeprazole 1 tablet/day, Controloc 40 mg/day and Neoral (Cyclosporine, schedule 75 mg-0-75mg; 50-0-50; 50-0-
50 then repeat).
The next 2 days, the evolution was stationary, the patient being still psychomotor agitated and experiencing the following psychiatric symptoms: psychotic anxiety, immediate echolalia, soliloquy, accelerated flow and rhythm of thoughts, logorrhea, visual and auditory hallucinations (“I see the devil, he took my voice and now he takes my liver too”). According to these symptoms, a new treatment schedule was proposed on 14.08.2014, Olanzapine being increased to 15 mg/day and Diazepam replaced with Lorazepam 3 mg/day maximum 6 mg/day. Zopiclone was withdrawn. During the day the patient continued to be psychomotor agitated, auto aggressive (continuously banged her head on the wall), having vivid visual and auditory hallucinations (“The devil is coming for me, I have to run”) which is why Olanzapine was changed to Haloperidol 30 drops (3 mg)/day with Midazolam i.m. added to the scheme in case of insomnia. Because the bruising still persisted on the arms, back and belly, Medrol was changed for Solu-Medrol perfusion starting in dose of 1g/day (14.08-17.08) decreased to 500 mg/day (18.08), 250 mg/day (19.08), 100 mg/day (20.08),
50 mg/day (21.08) which was continued with Medrol tablets 20 mg/day since 22.08.
During the next 4 days the psychomotor agitation decreased but the auditory and visual hallucinations still persisted, which is why Haloperidol was increased to 50 drops (5 mg/day) on 18.08, adding Romparkin 2 tablets/day and Lactulose syrup 3 doses/day at the recommendation of the gastroenterologist. The rest of the treatment scheme (Neoral, Omeprazole, Medrol, Siluvit F, Controloc) remained unchanged. The next day (19.08) the hallucinations were still persistent, Haloperidol being increased to 60 drops (6 mg/day).
Since 20.08.2014, the evolution of our patient started to improve. She became critic regarding her hallucinations and the psychotic anxiety diminished. The hallucinations disappeared completely on 25.08.2014 after 12 days of treatment with haloperidol (“I feel better, I don’t see or hear anything strange”), and the evolution was good until discharge, on 27.08.2014 after 15 days of hospitalization in the psychiatric unit. She was discharged with the following treatment scheme: Haloperidol 60 drops (6 mg)/day, Lorazepam (2 mg/day for 3 days then 1 mg/day for 7 days then only if needed), Romparkin 2 mg 3 tablets/day. At the recommendation of her surgeon, the scheme was completed with: Medrol 20 mg 1 tablet/day, Neoral (same scheme as during hospitalization), Omeprazole 20 mg 2 tablets/day, Lactulose 3 doses/day and Silivit F 1 tablet/day.
So far, the patient has been on the same treatment as after August 2014 discharge, her evolution was very good, without any psychiatric symptoms and she continued to work as a nurse. She comes for check-up every 2 months.
DISCUSSION:
In the described patient postoperative delirium was likely after the first psychotic episode because after surgery, delirium typically evolves immediately after emergence from general anesthesia or, after a lucid interval, in the first 72 hours [8]. This diagnosis was eliminated after the second psychotic episode, as the patient didn’t suffer another surgical intervention.
Another diagnosis we considered was psychotic episode induced by corticosteroids or immunosuppressive agents. Corticosteroids often induce psychiatric syndromes including depression, mania, psychosis, and delirium, known as “steroid psychosis”. Calcinurin inhibitors can cause neurologic and psychiatric side effects. Mild symptoms to severe complications can be found when the normal range of dose is administered. At the first episode this diagnosis could be possible because the psychotic symptoms evolved within a short period of time (after 3 days) from the transplant when the patient was in treatment with Solumedrol then with Tacrolimus which are known for their possible psychiatric adverse events. At the second episode the patient was in treatment with Cyclosporine which is less possible to cause psychotic symptoms. The most frequent psychiatric symptoms second to Cyclosporine treatment are cited to be anxiety a n d d e p r e s s i o n w i t h o u t p s y c h o t i c s y m p t o m s . [9,10,11,12,13]
Graft rejection was considered because of initial elevated bilirubin, but was excluded according to the results of investigations.
In chronic liver failure manifestations of encephalopathy are common and may reach from mild obtundation with
dementia and movement disorders to deep coma [14]. In the early phase of acute liver failure agitation, delusional ideas, and hyperkinesias are also common until coma finally ensues [15]. During the August 2014 admission the patient presented tremor of the arms which resembled
flapping tremor. Lab tests were performed and the diagnosis was excluded because of normal laboratory findings.
Hepatic artery thrombosis is a devastating complication after orthotopic liver transplantation often requiring revascularization or re- transplantation. It is associated with considerably increased morbidity and mortality. Acute cognitive dysfunction such as delirium or acute psychosis may occur after major surgery and may be associated with the advent of surgical complications [6, 16]. Abdominal ultrasonography and CT excluded this diagnosis.
Disseminated intravascular coagulation was another diagnosis taken in consideration because of the numerous ecchymoses on the arms, legs and belly but it was excluded because the coagulation tests were all normal. Intra-cranial tumors were excluded as a diagnosis because the cerebral CT didn’t reveal any pathological signs.
Schizophrenia was another discussed diagnosis because of her personal and family history, but the evolution between the two episodes and after the second one was good, so we also thought of a psychotic status after liver transplant.
CONCLUSIONS: Similar to other populations with chronic physical illnesses, patients with organ transplant are at elevated risk for psychiatric symptoms and diagnosable psychiatric disorders. Mood and anxiety-related disorders are the most common psychiatric illnesses observed both pre- and post transplant, although acute cognitive impairment and delirium are often seen shortly pre- transplant and preoperatively due to metabolic perturbations and the effects of surgery. Psychosis in transplant populations, although rare, is a significant concern because of its potential impact on health and well-being if not carefully managed [17]. Psychiatric complications of liver transplant can manifest in different ways and at various time points which makes detection and management challenging. Given the impact these have on patient and transplant outcome, it stresses the importance of vigilance, timely, adequate intervention and close collaboration between disciplines.
REFERENCES:
1. Tombazzi CR, Waters B, Shokouh-Amiri MH, Vera SR, Riely CA. Neuropsychiatric complications after liver transplantation: role of immunosuppression and hepatitis C.
Digestive diseases and sciences. 2006 Jun; 51(6):1079-81.
2.Campagna F, Biancardi A, Cillo U, Gatta A, Amodio P. Neurocognitive neurological complications of liver transplantation: a review. Metabolic brain disease.
2010 Mar; 25(1):115-24.
3. Fukunishi I, Sugawara Y, Takayama T, Makuuchi M, Kawarasaki H, Surman OS. Psychiatric disorders before and after living-related transplantation. Psychosomatics. 2001 Jul -Aug; 42(4):337-43.
4. Stracciari A, Guarino M. Neuropsychiatric complications of liver transplantation. Metabolic brain disease. 2001 Jun; 16(1-2):3-11.
5. Fukunishi I, Sugawara Y, Takayama T, Makuuchi M, Kawarasaki H, Surman OS. Association between pretransplant psychological assessments and posttransplant psychiatric disorders in living-related transplantation. Psychosomatics. 2002 Jan-Feb;43(1):49-54.
6. Krahn LE, DiMartini A. Psychiatric and psychosocial aspects of liver transplantation. Liver Transplantation, 2005; 10: 1157–1168.
7. Fukunishi I, Sugawara Y, Takayama T, Makuuchi M, Kawarasaki H, Surman OS, Psychiatric Disorders Before and After Living-Related Transplantation, Psychosomatics. 2001 Jul-Aug; 42(4):337-43.
8. Carmel Bitondo Dyer, MD; Carol M. Ashton, MD, MPH; Tom A. Teasdale, MPH, Postoperative Delirium.A Review of 80 Primary Data Collection Studies. Arch Intern Med. 1995; 155(5):461-465.
9. Sandeep Grover, Siddharth Sarkar. Journal of Clinical and Experimental Hepatology. December 2012, vol2(4): 382-394.
10.Wada K, Yamada N, Sato T et al. Corticosteroid – induced Psychotic and Mood Disorders. Psychosomatics 2001; 42:461- 466.
11. Patten SB, Neutel I. Corticosteroid – induced adverse psychiatric effects. Drug Safety 2000; 22:111-22.
12. Turjanski N, Lloyd G. Psychiatric side-effects of medications: recent developments. Advances in Psychiatric Treatment (2005), vol. 11, 58–70
13. Rojas- Estape H, Iclesias Rodriguez C, Murello LG. Hospitalized psychoses after liver transplantation. European Psychiatry 2011 vol26:395
14. Riordan SM, Williams R: Treatment of hepatic encephalopathy. N Engl J Med 1997, 337 (7): 473–479.
15. Lee WM: Acute liver failure. N Engl J Med 1993; 329 (25): 1862–1872.
16. Goralczyk A, Meier V, Ramadori G, Obed A, Lorf T. Acute paranoid psychosis as sole clinical presentation of hepatic artery thrombosis after living donor liver transplantation. BMC Surgery 2010 10.1186/1471- 2482-10-7
17. Sadock BJ, Sadock VA. Psychological Factors Affecting Medical Condition and Psychosomatic Medicine. Kaplan and Sadock’s Synopsis
of Psychiatry: Behavioral Sciences/Clinical Psychiatry. Philadelphia: Lippincott Williams and Wilkins, 2003, 849-850
***
Table 1. Evolution of the abnormal blood parameters.