PSYCHOPHARMACOLOGICAL POINTS OF REFERENCE IN PERSONALITY DISORDERS THERAPY FROM DSM-5 PERSPECTIVE
Abstract
Trăsăturile maladaptative de personalitate, care sunt exprimate de comportament, au constituit întotdeauna o problemă majoră în psihiatrie din cauza faptului că acestea reprezintă o sursă de suferință personală și colectivă. Impulsivitatea, anxietatea, labilitatea emoțională, excentricitatea sunt doar o parte din trăsăturile patologice care sunt externalizate prin comportamente care sunt considerate urgențe psihiatrice, cum ar fi hetero-agresivitatea și auto-agresivitatea. În afară de tratamentul psihoterapeutic, care este considerat tratamentul de elecție în aceste tulburări, tratamentul psihofarmacologic este încă în curs de dezbatere. Indicatiile acestuia se referă la componenta biologică a personalității dominata de trăsături temperamentale. Cloninger descrie temperamentul ca "nucleul emoțional" de personalitate și demonstrează că această componentă a personalității are o bază biologică, sugerând astfel intervențiile psihoterapeutice in tulburările de p e r s o n a l i t a t e . A c e s t s t u d i u d e s c r i e e f e c t u l psihofarmacologic și rolul acestuia asupra trăsăturilor de personalitate patologice și reunește cele mai multe atribute ale unei meta-analize. În același timp, studiul este adaptat la modelul personologic alternativă a DSM 5.
The personality disorder (PD) is defined in DSM 5 (Diagnostic and Statistical Manual of Mental Disorders) as an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture. It is pervasive and inflexible, its onset can be traced back to adolescence or early adulthood, is stable and of long duration and leads to distress or impairment (1).
As a result personality disorders are accompanied permanently by an adaptive deficiency of variable intensity and represent a constant source of suffering for the individual and for those next to him. In order to understand the pharmacodynamic and pharmacokinetic particularities of pharmacological medications in PD, we must begin with the biological component of the personality’s structure. Robert Cloninger proposes a system centered on three levels: temperament, character and the psyche (2). The three levels are defined based on three types of memory (Table 1.)
Temperament (“the emotional core” of personality) implies procedural memory, adjusted through the circuits of the cortico-striato-limbic system. Character (conceptual core of personality) is related to semantic memory, that implies more complex cognitive functions of abstracting and symbolization (3, 4, 5). Psychism – is related to episodic memory and implies the sole human process of symbolic invention, process that leads to the invention of art, science and spirituality (3, 4, 5).
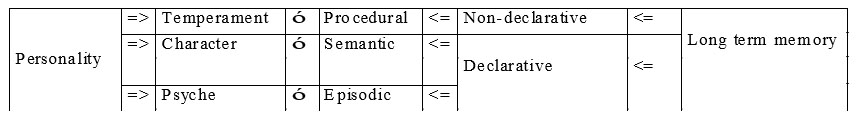
Table 1. The relationship between memory and personality: temperament is related to procedural memory, character to semantic memory, and the psyche to episodic memory
As mentioned above temperament, the biological component of personality, is related to the neurotransmitters’ functioning and implicitly easily influenced by the psychopharmacologic products.
Novelty seeking is a domain of temperament regulated by dopamine and is responsible for behavioral activation. H a r m a v o i d a n c e i s r e l a t e d t o s e r o t o n e r g i c neurotransmission. Studies on animals show that ascending serotonergic projections from the dorsal raphe nucleus inhibit dopaminergic nigrostriatal neurons, assuring this way the behavioral inhibition that is characteristic to this domain (6). Reward dependence depends on the noradrenergic connections of the cerulean nucleus with the thalamus and the temporal lobe, being responsible for the social behavior of the person (6). Persistence is a temperamental domain that depends on the hippocampal-striatal glutamatergic projections and which assure the transformation of behavioral inhibition caused by punishment into behavioral activation by anticipation of reward.
The symptoms related to temper are in a close relation with harm avoidance, impulses control and aggressiveness with novelty seeking, emotional and social detachment with reward dependence, and psychotic symptoms and cognitive distortions are related to persistence (7).
Any therapeutic approach of PD must start from the assessment of risk and benefit relation. Thus, we shall not resort to psychopharmacologic treatment in case of mild personality disorders, without maladaptive traits that would lead to self-aggressive and hetero-aggressive behaviors or when the patient’s functioning in roles is satisfying.
Patients’ compliance is another factor that influences directly the therapeutic success. Unfortunately, patients with moderate and severe personality disorders, who do not have psychotic symptoms or of aggressiveness outside the family, do not arrive at the psychiatric service because of the ego-syntonicity and the poor value of cooperativeness and reward dependence. If they get to benefit of psychopharmacologic treatment, chances that these patients respect the recommendations are very scarce.
The most studied personality disorder is the borderline personality disorder (BPD), followed by the schizotypal personality disorder (SPD) and by the rest of Cluster B personality disorders. Personality disorders that are characterized by novelty seeking and the ones with high reward dependence, these are the patients who end up benefiting of the psychopharmacologic treatment. Borderline personality disorder is the most severe personality disorder because the Self reaches an emphatic adverse patterning, and the diffused Self image causes extreme suffering to the individual.
T h e m e d i c a t i o n s u s e d i n t h e psychopharmacologic treatment of PD are antipsychotics, antidepressants, antiepileptics and anxiolytics.
Typical antipsychotics, in small doses, have effect on the psychotic symptoms and on the cognitive non-psychotic ones. It has been demonstrated that these medications may be beneficial also concerning the affective and behavioral symptoms (Table 2.).
These studies have proven also another aspect of the psychopharmacologic treatment of PD: lack of compliance to treatment. In case of typical antipsychotics the explanation being the side effects of these medications: aggravation of affective and cognitive negative symptoms by inhibition of the mesolimbic and mesocortical systems, the appearance of extrapyramidal symptoms, hyperprolactinemia, sedation, blurry vision, mouth dryness, orthostatic hypotension, akathisia, tardive dyskinesia.
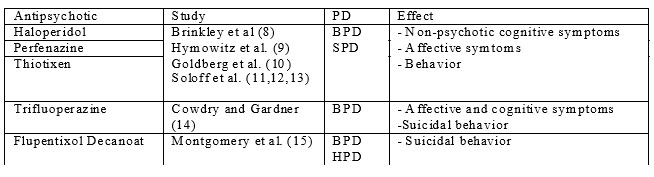
Table 2. The effect of typical antipsychotics in psychopharmacologic treatment of personality disorders. PD= Personality Disorder; BPD = Borderline Personality Disorder; SPD = Schizotypal Personality Disorder; HPD=Histrionic Personality Disorder
Along with the appearance of atypical a n t i p s y c h o t i c s a n e w c h a p t e r o p e n e d i n psychopharmacology and hence in PD treatment (Table 3). These medications, apart from their antidopaminergic effect, they also have an antiserotonergic effect (except for atypical antipsychotics – partial agonists of dopamine) that reduces the pro- extrapyramidal and hyperprolactinemic effect of nigrostriatal respectively, tuberoinfundibular hypodopamine.
In case of atypical antipsychotics the most important side effects are the cardiometabolic ones and gaining weight, especially in case of clozapine and olanzapine.
The antidepressants play an important role in the treatment of affective symptoms, impulsivity and affective lability of PD (Table 4.). It has been proved an e l e v a t e d e f f i c i e n c y o f m o n o a m i n e o x i d a s e inhibitors (MAOI) and selective serotonine reutake inhibitors(SSRI), the latter having less side effects as to MAOI.
Affective lability and impulsivity from PD have led to the introduction of antiepileptics medications in their medicamentary treatment (Table 5.). Thus, impulsivity, aggressiveness and affective lability of antisocial and borderline PD may respond to antimanic treatment. Lamotrigine seems to have a mood stabilizer effect more efficient in type I bipolar disorder besides the manic and depressive episodes (31) and possibly also in the case of affective lability encountered in borderline personality disorder. In the case of the mood in PD, lithium salts have a predominantly antimanic effect, and lamotrigine has a predominantly antidepressive effect (7).
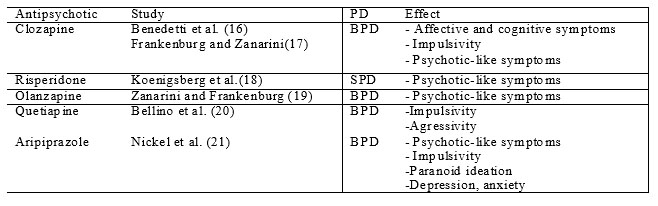
Table 3. The effect of atypical antipsychotics in psychopharmacologic treatment of personality disorders. PD= Personality Disorder; BPD = Borderline Personality Disorder; SPD = Schizotypal Personality Disorder
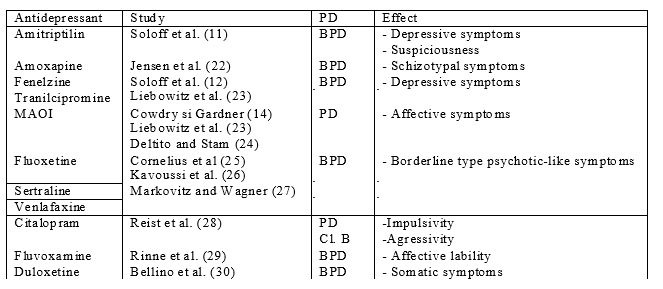
Table 4. The effect of antidepressants in psychopharmacologic treatment of personality disorders. PD= Personality Disorder; BPD = Borderline Personality Disorder; Cl. B = Cluster B Personality Disorder; MAOI = monoamine oxidase inhibitors
Benzodiazepines through their anxiolytic effect would have a beneficial effect in personality disorders of Cluster B and C, but they must be prescribed with caution because of the addiction they cause. Clonazepam for its anxiolytic and anticonvulsivant effect is preferable (46).
In 2001 APA has published a guide for BPD treatment (47). The first line treatment is the psychotherapeutic one, and the psychopharmacologic one as an adjunct treatment. I n t h i s g u i d e t h e r e c o m m e n d a t i o n s f o r t h e psychopharmacologic treatment of BPD are elaborated based on three algorithms that combat affective symptoms, a series of impulsive symptoms and cognitive- perceptual ones. Thus, for affective symptoms it is recommended SSRI alone or in combination with a neuroleptic and clonazepam which, if has no effect, it is changed with MAOI or mood stabilizers or with a combination of these. For impulsive symptoms, it is started with SSRI to which are added neuroleptics and mood stabilizers or MAOI, after which it is passed to an atypical antipsychotic, if the initial treatment did not function. The algorithm for cognitive-perceptual symptoms treatment starts with typical or atypical antipsychotics to which is added SSRI in case of coexisting affective symptoms, combination which is replaced by clozapine in case of its inefficiency.
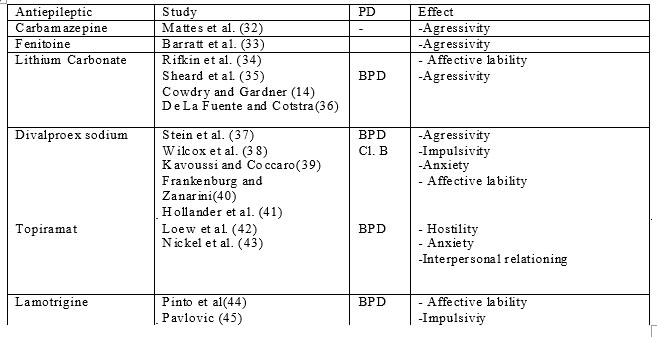
Table 5. The effect of antiepileptics in psychopharmacologic treatment of personality disorders. PD= Personality
Disorder; BPD = Borderline Personality Disorder; Cl. B = Cluster B Personality Disorder
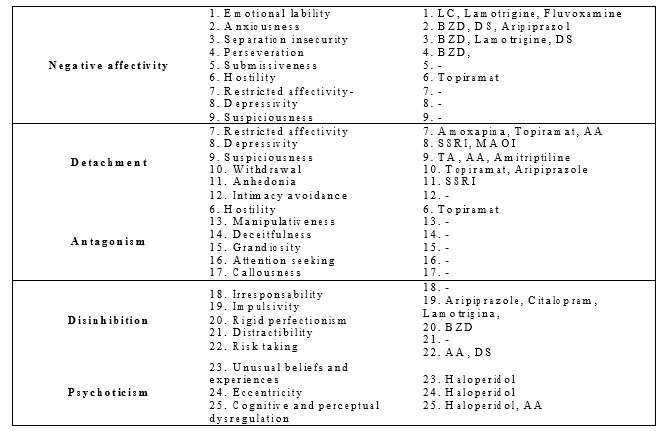
Table 6. Domains and facets of DSM V alternative model and the medication association variant proposed by our study group. LC=Lithium Carbonate; BZD=Benzodiazepines; DS=Divalproex Sodium; AA=Atypical Antipsychotics; SSRI= selective serotonine reuptake inhibitors; MAOI= monoamine oxidase inhibitors; TA= Typical Antipsychotics
In the psychopharmacology treatment of personality disorders, DSM-5 categorical system does not offer us too much help because it offers concrete information about pathological traits of the patient. The DSM-5 alternative system, that derives from the big five model, by its dimensional character is a good basis for future studies and to elaborate certain therapeutic strategies in PD.
This model contains five domains, each with 3-9 facets (1). Some facets belong to several domains (Hostility is a facet of the Negative Affectivity domain and of Antagonism domain), so there is an overlapping. The Flat Affectivity Facet – of the Negative Affectivity domain is in fact the opposite pole of this trait (in table indicated by a minus) to avoid overcharging the model with too many traits (Table 6.).
There are not any recent studies yet dedicated to the correspondents among the five described domains and the psychopharmacologic medications.
We propose a variant of medication associations that applies to domains on the whole and when possible to several of their composing facets. Clinical practice will confirm or infirm us the usefulness of the proposed strategy. This would be also a well certified support for psychotherapeutic interventions also.
Any of the responsive variants to haloperidol opens the path of using atypical antipsychotics that have effect on dopamine.
Traits which are allocated to self-esteem and individual Super ego seem to be difficult to integrate in this psychopharmacologic strategy.
REFERENCES
1.APA. DSM – Diagnostic and statistical manual of mental disorders – fifth edition. Washington DC: American Psychiatric Publishing, 2013.
2.Lăzărescu M, Nireştean A. Tulburările de personalitate. Iasi: Editura Polirom, 2007.
3.Cloninger CR. The temperament and character inventory (TCI): A guide to its development and use. St. Louis, MO: Center for Psychobiology of Personality: Washington University, 1994.
4.Cloninger CR, Svrakic DM, Pryzbeck TR. A psychobiological model of temperament and characters. Archives of General Psychiatry, 1993.
5.Cloninger CR. Feeling Good. The Science of Well-Being. Oxford: Oxford University Press, 2004.
6.Sadock BJ, Sadock VA, Ruiz P. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry, 9th Edition. New York: Lippincott Williams and Wilkins, 2009.
7.Tasman A, Kay J, Lieberman JA, First MB, Maj M. Psychiatry, Third Edition. Chichester: John Wiley and Sons, 2008.
8.Brinkley JR, Beitman BD, Friedel RO. Low dose neuroleptic regimes in the treatment of borderline patients. Archives of General Psychiatry 1979;36: 319-326.
9.Hymowitz P, Frances A, Jacobsberg LB, Sickles M, Hoyt R. Neuroleptic treatment of schizotypal personality disorders. Comprehensive Psychiatry 1986;27: 267–271.
10.Goldberg SC, Shulz SC, Shulz PM et al. Borderline and schizotypal personality disorders treated with low dose thiothixene versus placebo. Archives of General Psychiatry 1986;43: 680–686.
11.Soloff PH, George A, Nathan RS et al. Progress in pharmacotherapy of borderline disorders: a double blind study of amitriptyline, haloperidol and placebo. Archives of General Psychiatry 1986;43: 691–697.
12.Soloff PH, Cornelius JR, George A et al. Efficacy of phenelzine and haloperidol in borderline personality disorder. Archives of General Psychiatry 1993;50: 377-385.
13.Cornelius JR, Soloff PH, Perel JM et al. Continuation pharmacotherapy of borderline personality disorder with haloperidol and phenelzine. American Journal of Psychiatry 1993;150: 1843–1848.
14.Cowdry R, Gardner DL. Pharmacotherapy of borderline personality disorder: alprazolam, carbamazepine, trifluoperazine and tranylcypromine. Archives of General Psychiatry 1988;45: 111–119.
15.Montgomery SA, Montgomery D. Pharmacological prevention of suicidal behaviour. Journal of Affective Disorders 1982;4: 291–298.
16. Benedetti F. Sfortizini L, Colombo C et al, Low dose clozapine in acute and continuation treatment of severe borderline personality disorder. Journal of Clinical Psychiatry 1998;59: 103–107.
17.Frankenburg FR, Zanarini MC. Clozapine treatment of borderline patients: a preliminary study. Comprehensive Psychiatry 1993;34: 402–405.
18.Koenigsberg HW, Reynolds D, Goodman M et al. Risperidone in the treatment of schizotypal personality disorder. Journal of Clinical Psychiatry 2003;64: 628-634.
19.Zanarini MC, Frankenburg FR. Olanzapine treatment of female borderline personality disorder patients: a double-blind, placebo- controlled pilot study. Journal of Clinical Psychiatry 2001;62: 849–854.
20.Bellino S1, Paradiso E, Bogetto F. Efficacy and tolerability of quetiapine in the treatment of borderline personality disorder: A pilot study. J Clin Psychiatry 2006;67(7):1042-1046.
21.Nickel MK, Muehlbacher M, Nickel C et al. Aripiprazole in the Treatment of Patients With Borderline Personality Disorder: A Double- Blind, Placebo-Controlled Study. Am J Psychiatry 2006;163(5): 833- 838.
22.Jensen HV1, Andersen J. An open, noncomparative study of amoxapine in borderline disorders. Acta Psychiatrica Scandinavica 1989;79(1): 89-93.
23.Liebowitz MR, Fyer AJ, Gorman JM, Campeas R, Levin A. Phenelzine in social phobia. J Clin Psychopharmacol 1986;6(2): 93-98.
24.Deltito JA, Stam M. Psychopharmacological treatment of avoidant personality disorder. Comprehensive Psychiatry 1989;30(6): 498-504.
25.Cornelius JR1, Soloff PH, Perel JM, Ulrich RF. Fluoxetine trial in borderline personality disorder. Psychopharmacology Bulletin 1990;26(1): 151-154.
26.Kavoussi RJ1, Liu J, Coccaro EF. An open trial of sertraline in personality disordered patients with impulsive aggression. Journal of Clinical Psychiatry 1994;55(4): 137-141.
27.Markovitz PJ, Wagner C. Venlafaxine in the treatment of borderline personality disorder. Psychopharmacology Bulletin 1995;31: 773–777.
28.Reist C1, Nakamura K, Sagart E, Sokolski KN, Fujimoto KA. Impulsive aggressive behavior: open-label treatment with citalopram. Journal of Clinical Psychiatry 2003;64(1): 81-85.
29.Rinne T, van den Brink W, Wouter L, van Dyck R. SSRI treatment of borderline personality disorder: a randomized, placebo-controlled clinical trial for female patients with borderline personality disorder. American Journal of Psychiatry 2002;159: 2048– 2054.
30.Bellino S1, Paradiso E, Bozzatello P, Bogetto F. Efficacy and tolerability of duloxetine in the treatment of patients with borderline personality disorder: a pilot study. Journal of Psychopharmacology 2010;24(3): 333-339.
31.Stahl S.M. Stahl’s Essential Psychopharmacology. Neuroscientific Basis and Practical Applications. Fourth Edition. New York: Cambridge University Press 373, 2013.
32.Mattes JA. Comparative effectiveness of carbamazepine and propranolol for rage outbursts. The Journal of Neuropsychiatry and Clinical Neuroscience 1990;2(2): 159-164.
33.Barratt ES1, Stanford MS, Felthous AR, Kent TA. The effects of phenytoin on impulsive and premeditated aggression: a controlled study. Journal of Clinical Psychopharmacology 1997;17(5): 341-349.
34.Rifkin A, Quitkin F, Carrillo C, Blumberg AG, Klein DF. Lithium Carbonate in Emotionally Unstable Character Disorder. Archives of General Psychiatry 1972;27(4): 519-523.
35.Sheard MH, Martin JL, Bridges CI et al. The effect of lithium on unipolar aggressive behaviour in man. American Journal of Psychiatry 1976;133: 1409-1413.
36.De La Fuenta JM, Lostra F. A trial of carbamazepine in borderline personality disorder. European Neuropsychopharmacology 1994;4: 479–486.
37.Stein DJ1, Simeon D, Frenkel M, Islam MN, Hollander E. An open trial of valproate in borderline personality disorder. The Journal of Clinical Psychiatry 1995;56(11): 506-510.
38.Wilcox JA. Divalproex sodium as a treatment for borderline personality disorder. Annals of Clinical Psychiatry 1995;7(1): 33-37.
39.Kavoussi RJ, Coccaro EF. Divalproex sodium for impulsive aggressive behavior in patients with personality disorder. The Journal of Clinical Psychiatry 1998;59(12): 676-680.
40.Frankenburg FR, Zanarini MC. Divalproex sodium treatment of women with borderline personality disorder and bipolar II disorder. A double-blind placebocontrolled pilot study. The Journal of Clinical Psychiatry 2002;63: 442-446.
41.Hollander EI, Tracy KA, Swann AC et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology 2003;28(6): 1186-1197.
42.Loew THI, Nickel MK, Muehlbacher M et al. Topiramate treatment for women with borderline personality disorder: a double-blind, placebo- controlled study. Journal of Clinical Psychopharmacology 2006;26(1): 61-66.
43.Nickel MK, Nickel C, Mitterlehner FO et al. Topiramate treatment of aggression in female borderline personality disorder patients: a double- blind, placebo-controlled study. The Journal of Clinical Psychiatry
2004;65(11): 1515–1519.
44.Pinto OCI, Akiskal HS. Lamotrigine as a promising approach to borderline personality: an open case series without concurrent DSM-IV major mood disorder. Journal of Affective Disorders 1998;51(3): 333- 343.
45.Pavlovic ZM. Lamotrigine for the Treatment of Impulsive Aggression and Affective Symptoms in a Patient with Borderline Personality Disorder Comorbid with Body Dysmorphic Disorder. The Journal of Neuropsychiatry and Clinical Neurosciences 2008;20: 121- 122.
46.Freinhar JP, Alvarez WA. Clonazepam: a novel therapeutic adjunct. International Journal of Psychiatry in Medicine 1986;15(4): 321-328.
47.American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. American Journal of Psychiatry 2001;158(1-2): 1-52.
***




