LIPIDS, CHOLESTEROL AND SUICIDE RISK IN A ROMANIAN BIPOLAR POPULATION
Abstract
Introduction: Suicide rate in bipolar patients is one of the highest among psychiatric disorders. There are few biological markers linked to suicide risk and recent literature has focused on the relationship between lipid profile and suicidality. Objectives: This study aims to find if there is a link between the lipid profile of bipolar patients from a Romanian population and the risk of suicide. Method: We initially included 75 patients with ages between 18 and 65 years with a documented diagnosis of bipolar I disorder, confirmed by applying the Mini- International Neuropsychiatric Interview (MINI). We split them by their results on the Romanian version of the Columbia Suicide Severity Rating Scale (C-SSRS) into: “severe suicide attempts” group (N=11, 15,7%) and patients that never had a suicide attempt (N=46, 65.7%). There were also 13 patients (18.5%) in the “mild suicide attempts” group which we excluded from the analysis. In addition, various lab data have been collected: total Cholesterol, HDL Cholesterol, LDL Cholesterol and Triglycerides. Results: The mean age of the included patients was 44.28 (± 11.38) years, with the majority (58.7%) being female. Most of our patients were in a manic episode (N = 39, 52.0%), 16 (21.3%) were in a depressive episode, 15 (20.0%) were in remission and 5 (6.7%) were in a mixed episode. The number of total lifetime suicide attempts in our cohort was 24 (34.3%). We found no statistically significant difference between the suicidal and non- suicidal group regarding socio-demographic factors, treatments or lipid profile. The only statistically significant result (p=.031) was a higher level of LDL-cholesterol (148.2 mg/dl) in the suicide attempts group compared to non-suicide group (121.6 mg/dl). Conclusions: We found a positive association between LDL-cholesterol and suicide attempts, but more studies are needed in order to clarify the link between lipid profile and suicide attempts in patients diagnosed with bipolar disorder. It would be of utmost importance for clinicians if a quantifiable, biological marker could be linked to an increased risk of suicide.
INTRODUCTION
The World Health Organization (WHO) states that in 2008, 2.5 out of 1000 persons died of self-inflicted injuries and with approximately 1 million people (worldwide) dying each year by taking their own lives it can be considered it a major public health problem. Among psychiatric afflictions, bipolar disorder is on the higher end regarding suicidality with 3,4 – 14% deaths and 23–26% attempts. Another study estimates that a quarter to half of all bipolar patients will attempt suicide at some point during their life and 8% to 19% will complete suicide. Some of the factors (3) that raise the risk of suicide deaths in bipolar disorder are: male gender, older age (higher ratio of death/attempts), having more depressive, mixed or manic states with psychotic features, history of suicide attempts or suicide deaths in the family and the presence of psychosocial precipitants.
The presence of metabolic syndrome (5) was also associated with higher rates of suicide attempts. Metabolic syndrome is defined (6) as a combination of at l e a s t 3 o f t h e f o l l o w i n g : a b d o m i n a l o b e s i t y, hypertriglyceridemia (≥ 150 mg/dL), low HDL- cholesterol, high blood pressure and high fasting glucose. One factor (7) considered to impact suicidal behaviour and offer a subsequent explanation for the influence of metabolic syndrome, is dietary lipid intake. This hypothesis came to attention because of two meta- analyses (8,9) which showed that statins did not increase non-illness mortality and that non-statin treatments raised mortality due to suicide, accidents or trauma. Other findings (10) showed that lower total cholesterol and LDL-C levels were associated with higher risk of suicidality, possibly moderated by lower plasma levels of polyunsaturated fatty acids (PUFAs). Lower n3-PUFAs were observed in patients diagnosed with depression compared to healthy controls (11) and were also associated with the presence of impulsive/aggressive behaviour, important findings since both are considered suicidal risk factors(12,13).
Daray et al. (7) explained that lipids affect suicidal behaviour by disrupting the lipid rafts of the cellular membrane which causes alterations in serotonergic neurotransmission, low activation and dimerization of Toll-like Receptors (TLR), altering peroxisome proliferator-activated receptors (PPARs) and downregulating the nuclear factor kappa light chain enhancer of activated B cells (NF-κB) thus raising the inflammatory status. Besides the direct effect of serotonin in modulation of suicide behaviour (13), the rest of the pathways might influence suicidality via raising systemic inflammation, an effect also supported by the anti- inflammatory effects of statins which show a lower tendency of suicide(9).
The role of serum lipids of bipolar patients and their risk of suicide has been recently studied but with mixed results. Some studies (14,15) found a significant association between low levels of cholesterol and triglycerides and increased suicide attempts while others ––––(1621) found no association. A meta-analysis (17) of 11 studies, showed no associations between total cholesterol, LDL-cholesterol or triglyceride levels and suicide attempts in bipolar patients. Interestingly, one study (22) of 80 bipolar patients found a positive association between high levels of cholesterol and suicide
attempts. It has been hypothesized (23,24) that suicidal behaviour could in fact be influenced by violence, aggression, hostility and impulsivity, all of which associate with low levels of cholesterol. One hypothesis suggests that low cholesterol levels are associated with low membrane microviscosity of central nervous cells and diminished exposure of serotonin to membrane receptors (25). Secondary to receptor disfunction, there is an altered suppresion of aggressive and impulsive behaviour of susceptible individuals, hypercholesterolemia being proposed as a protective factor for suicide behaviour.
The purpose of our study is to observe if plasma lipid levels are associated with a history of serious suicide attempt in a Romanian bipolar population. Because of the present conflicting data about lipid profile and suicide in bipolar patients every contribution could shed new light regarding this topic. Also, given the high risk of suicide in
bipolar patients (4), finding a biological factor that not only could predict suicide attempts but also be modified through pharmacological means could be a breakthrough.
MATERIALS AND METHOD
The material and methods were been described lengthy in other paper (26) therefore, the information about the study will be provided in short.
The study protocol was designed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the “Prof. Dr. Alexandru Obregia” Clinical Psychiatry Hospital in Bucharest, Romania. All the patients admitted to the “Prof. Dr. Alexandru Obregia” Clinical Psychiatry Hospital with a documented diagnosis of bipolar I disorder between June 1st, 2015 and February 1st, 2016 were asked to participate in the present study. They were presented with an approved informed consent form, they were given enough time to read, and all of their concerns were addressed before signing the form.
The inclusion criteria were represented by those of between 18 and 65 years of age with a documented diagnosis of bipolar I disorder, confirmed by applying the Mini-International Neuropsychiatric Interview (MINI) (27). The exclusion criteria were: the presence of any psychiatric disorder that, in the investigators’ opinion, could interfere with the clinical assessments (e.g. organic mental disorders, mental retardation, etc.), any significant physical disability, severe or uncontrolled medical conditions, and maternal status (pregnancy or postpartum).
The MINI is a short, structured diagnostic interview based on the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV). In order to confirm the diagnosis of bipolar I disorder among the participants included in the study, we used the Romanian translated version 6.0.0 of the MINI.
The Romanian version of the Columbia Suicide Severity Rating Scale (C-SSRS), a semi-structured interview, was used for assessing suicide ideation and behaviour (28). The first subscale, the suicidal ideation scale, is a 5-point ordinal scale ranging from 1 (wish to be dead) to 5 (active suicidal ideation with specific plan and intent). Patients who denied suicidal ideation received a zero score. Suicidal ideation intensity assessment is comprised of five items (i.e., frequency, duration, controllability, deterrents, reasons for suicidal thoughts), each rated on an ordinal scale. This subscale uses two different assessment periods (i.e. lifetime, past month). The second subscale, measuring suicidal behaviour, investigates interrupted, aborted and actual suicide attempts, as well as preparatory behaviour for a suicide attempt and non-suicidal self-injurious behaviour. Furthermore, actual suicide attempts (most recent/most lethal/initial) are assessed by an ordinal lethality subscale, which categorizes the medical consequences of actual suicide attempts on a scale from 0 (no physical damage) to 5 (death). The subscale additionally registers the number of attempts (actual, interrupted and aborted) and uses two distinctive assessment periods (lifetime and past year). There are 6 possible outcomes of the suicide attempt: 0.No physical damage or very minor damage (e.g. surface scratches)
1.Minor physical damage (e.g. lethargic speech; first- degree burns, mild bleeding)
2.Moderate physical damage; medical attention needed (e.g. conscious but sleepy, some burns; bleeding of major vessels)
3.Moderately severe physical damage; medically hospitalization and likely intensive care required (e.g. comatose with reflexes intact; thirst degree burns with less than 20% of body; extensive blood loss but can be recover; major fractures)
4.Severe physical damage: medical hospitalization with intensive care required (e.g. comatose without reflexes, third degree burns over 20% body; extensive blood loss with unstable vital signs; major damage to a vital area)
5.Death
The terms self-harm and suicide are often used together, and self-harm (such as low lethality overdose or self-inflicted lacerations) is an established risk factor for suicide (29). Nevertheless, it is important to acknowledge that self-harm is not necessarily synonymous with suicidal intent. In reality, most self-harm inflicts little actual harm and does not come to the attention of mental health
services. Because medical hospitalization well represents an indicator of severity of suicide attempt, we separated the 6 above possible outcomes of suicide attempt into 2 categories:
1.Mild suicide attempts (all cases that did not need medical hospitalization).
2.Severe suicide attempts (with high lethality, meaning all cases that needed medical hospitalization).
In addition, various lab data have been collected. In this paper we analysed: total Cholesterol, HDL Cholesterol, LDL Cholesterol and Triglycerides.
STATISTICALANALYSIS
The statistical analysis was performed using IBM SPSS 20. Except for: age of debut (Shapiro-Wilk .293), total plasma cholesterol (Shapiro-Wilk .483), HDL-
cholesterol (Shapiro-Wilk .270) and LDL-cholesterol (Shapiro-Wilk .802), all other continuous variables analysed in our paper are non-normally distributed. Categorical data was analysed with chi-square test. Continuous normally distributed data was analysed with t- test. Continuous non normally distributed data was analysed with Mann-Whitney test. All statistically significance alpha value was set at .05.
RESULTS
Seventy-five bipolar patients were initially included in this study, with a mean age of 44.28 ± 11.38 years. Of the total number of participants, 58.7% were females. Most of our patients were in a manic episode (N =
39, 52.0%), 16 (21.3%) were in a depressive episode, 15 (20.0%) were in remission and 5 (6.7%) were in a mixed episode. The number of total lifetime suicide attempts in our cohort was 24 (34.3%). There were 11 patients (15,7%) in the “severe suicide attempts” group and 46 (65.7%) patients that never had a suicide attempt. There were also 13 patients (18.5%) in the “mild suicide attempts” group (patients that did not necessitate hospitalization) that were excluded from analysis.
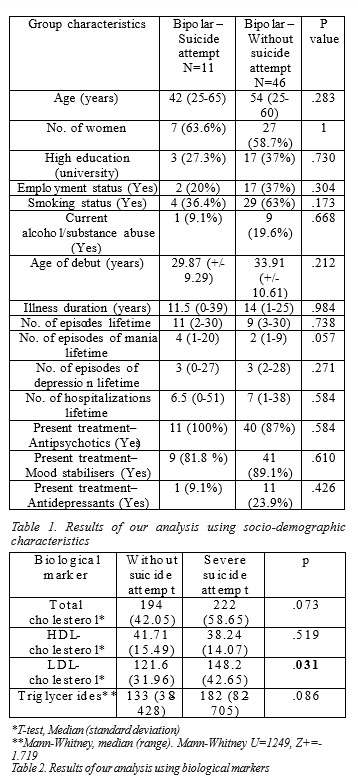
We compared bipolar patients from the “severe suicide attempts” group with bipolar patients without suicide attempts. Results of this comparison is presented in Table 1. Results of the comparison using biological markers mentioned above are presented in Table 2.
DISCUSSION
When comparing the median values of lipid markers between the two groups, the only statistically significant result was for the LDL-cholesterol (p=.031), with higher levels in the suicidal group (148.2 mg/dl, SD=42.65, respectively 121.6 mg/dl, SD=31.96 in the non-suicidal group). Our result is in opposition with some studies (7,10,16,17), which show either a negative or no association between plasma lipid levels and suicide attempts.
Studies point out a link ‘(30,31) between obesity (defined as BMI>25) and increased suicide attempts in bipolar patients but few studies have gone beyond that to see if obesity is just a moderator. One explanation for this comes from a study (32) that found an association between suicide attempts and both binge eating behaviour and binge eating disorder. Going further (33), after controlling for obesity, the presence of binge eating disorder was associated with suicidality, psychosis and mood instability. It is possible that binge eating and impulsivity traits could be a determining risk factor for increased suicide moderated by obesity and lipid profile of bipolar patients.
What is more, leptin, a hormone known to
regulate energy homeostasis (34), has been associated both positively (35) and negatively (36) with depression and suicidality. Regarding lipid metabolism, low levels of leptin or leptin resistance cause high levels of cholesterol, triglycerides and LDL-cholesterol (34) which could explain our result.
Clearly, more studies are needed to clarify the causality link between lipid metabolism, obesity and suicide risk. By exploring this link, we could better understand suicidality in patients with bipolar disorder and, if proven to be true, we would have an easily traceable and modifiable biological marker that may influence these patients’ outcomes in a positive manner. What is more, we c o u l d , t h r o u g h b o t h p h a r m a c o l o g i c a n d n o n – pharmacologic (changes in life style through diet, physical activity, smoking cessation) means start a suicide prevention strategy.
CONCLUSIONS
Our study showed a positive association between LDL-cholesterol and suicide attempts. At the moment, results in literature are mixed but with a tendency to show a link between lipid metabolism, affective disorders and suicidality.
Given the high incidence of suicide in bipolar disorder, it would be of the utmost importance for clinicians if a quantifiable, biological marker could be linked to an increased risk of suicide.
REFERENCES
1. Organization WH. Causes of death 2008: data sources and methods. Geneva World Heal Organ. 2011;
2. Suicide WHOP. A global imperative. World Heal Organ. 2014;
3. Schaffer A, Isometsä ET, Azorin JM, Cassidy F, Goldstein T, Rihmer Z, et al. A review of factors associated with greater likelihood of suicide attempts and suicide deaths in bipolar disorder: Part II of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. Aust N Z J Psychiatry. 2015;49(11):100620.
4. Marangell LB, Bauer MS, Dennehy EB, Wisniewski SR, Allen MH, Miklowitz DJ, et al. Prospective predictors of suicide and suicide attempts in 1,556 patients with bipolar disorders followed for up to 2 years. Bipolar Disord. 2006;8(5p2):56675.
5. Aas M, Etain B, Bellivier F, Henry C, Lagerberg T, Ringen A, et al. Additive effects of childhood abuse and cannabis abuse on clinical expressions of bipolar disorders. Psychol Med. 2014;44(8):165362.
6. Goodman DS, Hulley SB, Clark LT, Davis CE, Fuster V, LaRosa JC, et al. Report of the National Cholesterol Education Program Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults. Arch Intern Med. 1988;148(1):3669.
7. Daray FM, Mann JJ, Sublette ME. How lipids may affect risk for suicidal behavior. J Psychiatr Res. 2018;104(May).
8. Muldoon MF, Manuck SB, Matthews KA. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials.
Bmj. 1990;301(6747):30914.
9. Muldoon MF, Manuck SB, Mendelsohn AB, Kaplan JR, Belle SH. Cholesterol reduction and non-illness mortality: meta-analysis of randomised clinical trials. Bmj. 2001;322(7277):115.
10. Wu S, Ding Y, Wu F, Xie G, Hou J, Mao P. Serum lipid levels and suicidality: a meta-analysis of 65 epidemiological studies. J psychiatry Neurosci JPN. 2016;41(1):56.
11. Lin P-Y, Huang S-Y, Su K-P. A meta-analytic review of polyunsaturated fatty acid compositions in patients with depression. Biol Psychiatry. 2010;68(2):1407.
12. Teti GL, Rebok F, Rojas SM, Grendas L, Daray FM. Systematic review of risk factors for suicide and suicide attempt among psychiatric patients in Latin America and Caribbean. Rev Panam Salud Pública. 2014;36:12433.
13. Van Heeringen K, Mann JJ. The neurobiology of suicide. The Lancet
Psychiatry. 2014;1(1):6372.
14. Vuksan-Ćusa B, Marčinko D, Nad S, Jakovljević M. Differences in cholesterol and metabolic syndrome between bipolar disorder men with and without suicide attempts. Acta Neuropsychiatr. 2009;21(S2):669.
15. Ainiyet B, Rybakowski JK. Suicidal behaviour and lipid levels in u n i p o l a r a n d b i p o l a r d e p r e s s i o n . A c t a N e u r o p s y c h i a t r. 2014;26(5):31520.
16. Tsai S-YM, Kuo C-J, Chen C-C, Lee H-C. Risk factors for completed suicide in bipolar disorder. J Clin Psychiatry. 2002;
17. Bartoli F, Di Brita C, Crocamo C, Clerici M, Carrà G. Lipid profile and suicide attempt in bipolar disorder: A meta-analysis of published and unpublished data. Prog Neuro-Psychopharmacology Biol Psychiatry [ I n t e r n e t ] . 2 0 1 7 ; 7 9 ( J u n e ) : 9 0 5 . A v a i l a b l e f r o m : http://dx.doi.org/10.1016/j.pnpbp.2017.06.008
18. Ahmadpanah M, Haghighi M, Jahangard L, Borzoei S, Heshmati S, Bajoghli H, et al. No evidence for metabolic syndrome and lipid profile differences in patients suffering from bipolar I disorder with and without suicide attempts. Int J Psychiatry Clin Pract. 2015;19(3):16873.
19. Park S, Yi KK, Na R, Lim A, Hong JP. No association between serum cholesterol and death by suicide in patients with schizophrenia, bipolar affective disorder, or major depressive disorder. Behav Brain Funct. 2013;9(1):45.
20. Valtonen HM, Suominen K, Haukka J, Mantere O, Leppämäki S, Arvilommi P, et al. Differences in incidence of suicide attempts during phases of bipolar I and II disorders. Bipolar Disord. 2008;10(5):58896.
21. DAmbrosio V, Salvi V, Bogetto F, Maina G. Serum lipids, metabolic syndrome and lifetime suicide attempts in patients with bipolar disorder. Prog Neuro-Psychopharmacology Biol Psychiatry [Internet]. 2 0 1 2 ; 3 7 ( 1 ) : 1 3 6 4 0 .
A v a i l a b l e f r o m : http://dx.doi.org/10.1016/j.pnpbp.2011.12.009
22. Shakeri J, Farnia V, Valinia K, Hashemian AH, Bajoghli H, Holsboer- Trachsler E, et al. The relationship between lifetime suicide attempts, serum lipid levels, and metabolic syndrome in patients with bipolar disorders. Int J Psychiatry Clin Pract. 2015;19(2):12431.
23. Pozzi F, Troisi A, Cerilli M, Autore AM, Castro C Lo, Ribatti D, et al. Serum cholesterol and impulsivity in a large sample of healthy young men. Psychiatry Res. 2003;120(3):23945.
24. Golomb BA, Stattin H, Mednick S. Low cholesterol and violent crime. J Psychiatr Res. 2000;34(45):3019.
25. Alvarez JC, Cremniter D, Lesieur P, Gregoire A, Gilton A, Macquin- Mavier I, et al. Low blood cholesterol and low platelet serotonin levels in violent suicide attempters. Biol Psychiatry. 1999;45(8):10669.
26. Giurgiuca A, Nemes B, Sorina Schipor A, Caragheorgheopol A, Cozman D TC. Suicide risk is associated with low levels of platelet serotonin in bipolar I disorder. Rom J Leg Med. 2017;(25):20510.
27. Sheehan D V, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12(5):23241.
28. Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, et al. Columbia-suicide severity rating scale (C-SSRS). New York, NY Columbia Univ Med Cent. 2008;
29. Zahl DL, Hawton K. Repetition of deliberate self-harm and subsequent suicide risk: long-term follow-up study of 11 583 patients.
Br J Psychiatry. 2004;185(1):705.
30. Gomes FA, Kauer-SantAnna M, Magalhães P V, Jacka FN, Dodd S, Gama CS, et al. Obesity is associated with previous suicide attempts in bipolar disorder. Acta Neuropsychiatr. 2010;22(2):637.
31. Fagiolini A, Kupfer DJ, Rucci P, Scott JA, Novick DM, Frank E. Suicide attempts and ideation in patients with bipolar I disorder.
J Clin Psychiatry. 2004;65(4):50914.
32. Bobo W V., Na PJ, Geske JR, McElroy SL, Frye MA, Biernacka JM. The relative influence of individual risk factors for attempted suicide in patients with bipolar I versus bipolar II disorder. J Affect Disord [ I n t e r n e t ] . 2 0 1 8 ; 2 2 5 : 4 8 9 9 4 . A v a i l a b l e f r o m : http://dx.doi.org/10.1016/j.jad.2017.08.076
33. McElroy SL, Crow S, Biernacka JM, Winham S, Geske J, Barboza ABC, et al. Clinical phenotype of bipolar disorder with comorbid binge eating disorder. J Affect Disord. 2013;150(3):9816.
34. Prieur X, Tung YCL, Griffin JL, Farooqi IS, ORahilly S, Coll AP. Leptin regulates peripheral lipid metabolism primarily through central effects on food intake. Endocrinology. 2008;149(11):54329.
35. Pasco JA, Jacka FN, Williams LJ, Henry MJ, Nicholson GC, Kotowicz MA, et al. Leptin in depressed women: cross-sectional and longitudinal data from an epidemiologic study. J Affect Disord. 2008;107(13):2215.
36. Jow G-M, Yang T-T, Chen C-L. Leptin and cholesterol levels are low in major depressive disorder, but high in schizophrenia. J Affect Disord.
2006;90(1):217.
***



